
Mary Beth Kingston Executive Vice President and Chief Nursing Officer at
Advocate Health

Dominique Wells Chief Operating Officer at
Conduit Health Partners

Andrew Adams Co-Founder and Managing Partner at
Oak HC/FT
Greg Sloan Chief Purpose Officer and Co-Founder at
Go Beyond

Larina Burke Hyasynth Bio at
Laboratory Manager

Karen Correa Vice President and Head of Global Clinical Operations at
Takeda Pharmaceuticals

John D. Couris President & CEO at
Tampa General Hospital

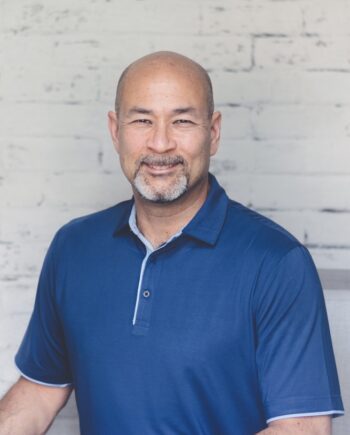
Hank Osowski Founding Member and Managing Partner at
Strategic Health Group LLC

John Lee Dumas Founder and Host at
Entrepreneurs on Fire

Fran Ayalasomayajula Founder and leader of Reach at
Reach

Sabrina Runbeck Cardiothoracic Surgeon, Peak Performance Coach and Speaker at
Sabrina Runbeck's Success System