Burnout is common among medical practitioners and healthcare workers. Add the strain of managing COVID19 to the mix, and you have a recipe for depression. How do you build resilience in your medical staff? That’s the topic for today’s interview with Chris Dimock and Carlos Arce of Elation.
Chris is the Founder and Carlos is the Organizational Development Consultant and Facilitator. They discuss how their company is helping organizations create healthy dynamics and improve performance through tailored approaches to bring joy back to the workplace. They also share how they leverage technology to optimize the coaching sessions in this pandemic season.
Please tune it to our exciting interview with Chris and Carlos!
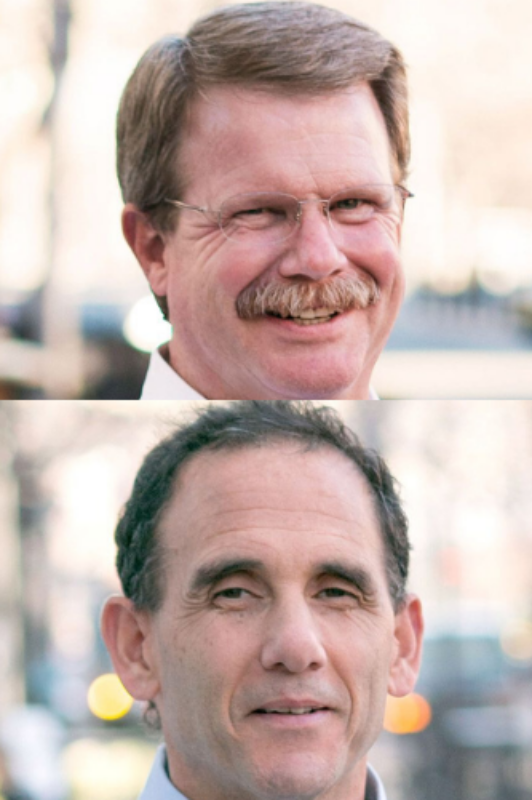
Chris Dimock
Chris is the founder of Elation and has always been interested in what drives improved human performance since his college days. A curiosity about developmental psychology expanded into a love for organizational development and the design of technologies that improve organizational performance. He was inspired to start Elation after a career in the tech industry. His passion for helping people through the use of innovative technologies transitioned into a calling to help people flourish by applying what we know from neurobiology and mindset research. Seeing the transformative benefits of this approach has only fueled his enthusiasm, and helped attract an extraordinary team of people who share in the mission.
Chris completed both his bachelor’s and master’s at Boston College.
Carlos Arce
Carlos has been highly successful as a keynote speaker, workshop presenter, and consultant. He works directly with many of the clients and organizations hired by Elation. He is a coach and teacher whose purpose is to inspire people to be better. He continually helps leaders and companies achieve outstanding business results while improving organizational culture and employee engagement.
Carlos finished his bachelor’s at Santa Clara University and his masters at the University of California, Los Angeles.
Building Resilience in Your Medical Staff with Chris Dimock and Carlos Arce of Elation was automatically transcribed by Sonix with the latest audio-to-text algorithms. This transcript may contain errors. Sonix is the best audio automated transcription service in 2020. Our automated transcription algorithms works with many of the popular audio file formats.
Saul Marquez:
Welcome back to the podcast, Saul Marquez here. And today I have the privilege of hosting Chris Dimmock and Carlos Arce. Both are at the outstanding company Elation. Chris is the founder and he’s been interested in what drives improved human performance since his days in college. A curiosity about developmental psychology expanded into a love for organizational development and the design of technologies that improve organizational performance. He was inspired to start Elation after a career in the tech industry. His passion for helping people through the use of innovative technologies transitioned into a calling to help people flourish by applying what they know from neurobiology and mindset research. Seeing the transformative benefits of his approach, it’s only fueled his enthusiasm and help attract an extraordinary team of people who share in the mission. Carlos Arce is the Organization of development consultant and facilitator at Elation, and he’s been highly successful as a keynote speaker, workshop presenter and consultant. He works directly with many of the clients and organizations hired by elation. He’s a coach and a teacher whose purpose is to inspire people to be better. He continually helps leaders and companies achieve outstanding business results while improving organizational culture and employee engagement. These are these are things that we all strive for in our businesses and in our in our organizations. And today, we’re going to dive into the work that they’re doing ambulation to help with the problem of physician burnout and the feeling of lack of community, those things that are so important and primary needs. And an even you think of Maslow’s hierarchy of needs. They’re there. They’re getting after it in a big way and have seen a lot of success. And I’m and I’m privileged to have both of them here with us today to talk about the work that they’re doing. So, Carlos and Chris, thanks so much for joining me on the podcast today.
Carlos Arce:
Saul, thanks for having us.
Saul Marquez:
Absolutely. So before we dive into the work of Elation, love to get a feel for what inspires both of you two to work within health care.
Chris Dimock:
Well, this is Chris. I have looked at the statistics on health care over the last several years and been absolutely amazed at the level at which turnout has become an issue among physicians and other medical personnel. You know, the studies have been fairly consistent that it’s around the 50 percent level of diagnosable symptoms of burnout, according to the W8 chose diagnosis spectrum. And so it is sort of a burning platform issue for health care in the United States. If you have physicians who are performing at less than their optimum ability, obviously impacts the quality of care outcomes for all people.
Carlos Arce:
Yeah. And Saul, I think that’s a great question. I had the privilege of actually spending 13 years of my career in health care and support presented at a title that some people find a little bit mystical called Chief Learning Officer for a portion of that time where you got it. I got a chance to really experience the industry on a daily basis, and to be honest with you. It was an extraordinary privilege to watch the kind of work that’s happening daily by nurses and doctors. And in my time there, I really got a chance to explore the cultural dynamics of how the interactions between professionals, how the interactions between administration and clinicians, although it kind of contributes to the general sense of the support and the affect of daily activity, right.. So in my case, I wasn’t necessarily brought in to address burnout, but I was really focused on how do you ultimate optimize performance of both individuals and the group. So I had a passion for health care from the very beginning when we started doing work with elation, seeing the results that we were accomplishing private sector with a lot of different kind of exploratory technologies and the combination of exploratory and proven methodologies. That’s when we thought, hey, we have something I think that can contribute to this or to this industry. That is, as Chris put, you know, dealing with some some pretty challenges and pretty daunting threats that happen on a regular basis. And how do we make sure we we give it to the folks who need it the most of it?
Saul Marquez:
Yes, it’s so fantastic. I mean, the problem is clear. And, you know, we we talk about the quadruple aim, that fourth one being clinician satisfaction, right and wellness. And so you guys are tackling it head on. If our providers aren’t healthy, then it’s going to be even harder to provide better outcomes for for for patients overall. And so let’s let’s dive into it. Guys, what is it that Elation is doing to add value to the provider ecosystem?
Carlos Arce:
Yes. I think I’ll take that on, Chris, Saul. And if you want a time and feel free to my what we’re doing is we’re looking at the problem in its most authentic form. We are addressing this as an organizational dynamic. We see that we know the pathway that clinicians have to take to become practitioners in this country. It is not easy. It is not for the faint of heart. So we actually often reference the notion that we take some of the most resilient humans on the planet and created an epidemic of burnout. And so if you’re honest about that statement and you have to acknowledge the systemic implications of that, what what’s happening when you put those people into this workplace that over time ends up eroding this amazing competency that they bring to the table? So that’s an important element because of our approach. And because of that focus, we see that there isn’t. This isn’t about fixing physicians and this isn’t about this direct cause and effect relationship that all this one thing is causing this dynamic for everybody. There is a local element to this that you’ve got to pay attention to. And then there is this combination of both the individual and the individual within this group and the system. So we’ve taken methodologies that are helpful for individuals like executive coaching that we know works and puts people in the right spot. We’ve taken this approach as we’ve learned from organizational development, when it comes to creating workplace cultural dynamics that are that are healthy and that are actually what we would call resilient in and of themselves. So this idea of organizational resilience, which involves group work and group interactions between the the key players, and we have kind of combined those to ultimately influence not only the individual themselves in a way to get them informed about what helps them or what actually contributes or undermines their own resilience, but also vesting in them as catalysts for change within that health care organization itself. We title our work physician informed organizational resilience pie or is our lack. But the idea is that they can invest in having people understand what’s going on. These are the people who need to invest in the practitioners. And let’s be honest about the fact we’re trying to actually shift this organization. So.
Saul Marquez:
I think that’s great. Yeah. Go ahead.
Chris Dimock:
Carlos is mentioning that a lot of the symptoms of burnout look similar across a different organization. It’s one of the things that we’ve learned is that it is really sort of the unique combination of the environmental impact within a particular organization with the particular care provider physician. And so one of the reasons that programmatic solutions don’t tend to work is that they sort of assume that there’s a plain vanilla solution that will address burnout for a broad group of people. And what we’ve discovered is that you really do need to have sort of a handcrafted approach so that you can help tease out the underlying systemic issues that are contributing to burnout in a way that you can actually help the physicians focus on addressing and remedying them.
Saul Marquez:
And that’s fascinating. And I think it’s an neat approach. I guess meat is not the word. It’s a it’s a it’s a well informed approach that that ties in things that work outside of health care, executive coaching, performance solutions. And you tie in with with a physician informed approach to the organization. Tell us what exactly you know makes you guys different than what’s available out there and why. You know, the listeners should think about considering you.
Carlos Arce:
That’s I think what we’ve done is tempted to acknowledge all of the things that are going on out there, making sure we build a methodology that is aligned to the science and the research of what creates resilience. And so what we want to do is we want to make sure that our efforts don’t end up running counter purpose to what a lot of places are already doing, whether they’re investing in things like physician satisfaction or the idea of physician leadership or the investments that people are making around safety and quality. This approach is designed to be able to complement those efforts. So we’ve taken that expertise that we’ve acquired from creating organizational change and moving systems and saying, OK, how would you design this in a way so that the first so that we don’t overwhelm people with another approach, build this in a way that actually positions the people who are doing the work to be successful. There’s really kind of three key areas for us that we’re that we’re wanting to focus on. One, we’re going to use a diagnostic. We’re going to assess are the change. And the shift was something that actually helps people understand the problem itself. So we actually have or we use a tool called the four core diagnostic from a company called Neuro Zone. That’s really just research what creates high performing individuals. And one of the core competencies of their four core competencies is that it assesses is resilience. So we’re using that on the front end, on the back end, so that not only are we be able to measure the right thing, but we’re also wanting the people who are completing this diagnostic to become a more aware of the little things that can make a huge difference for them. The other elements of this, of focusing on both as complementary individual and the group work that we talked about earlier, those have to have a ability to be able to interact with one another. So when we’re working with a group of clinicians and administrators, a cohort, they’re being they’re also receiving one eye, one executive coaching simultaneously. It’s happening kind of in parallel Right. because these changes are happening in all different ways that are unknown to us individually. I don’t know what it’s going to take for you to be in your best place. And you don’t know it’s going to take for me to be in my best place. Sometimes that will happen from being in my group and seeing the changes in the group and seeing that the system itself shifting. Some of that might have to be with some patterns that I’ve developed that have been kind of male maladaptive behaviors that over time I just figure it’s not that big of a deal. I’ll just suck it up and bear through the tough stuff. And we know that in the long run, that can take its toll on people. So our approach is just kind of blended interaction so that we can pay attention to the systemic shifts that are happening. And that, again, is intended to occur so that it complements whatever else an organization is invested in, whatever else they’re focusing on, like patient safety, like some of these key areas around the patient experience. We want to make sure that people don’t see this as a competing dynamic. This is a complementary intended to move the organization in the right direction.
Chris Dimock:
And I would also add that in this era of reduced contact, we do this over Zoom. And so it’s actually a very effective delivery methodology and the mission is often actually say that they preferred over doing Face-To-Face work. When we do the facilitated session, you might touch on that a little bit.
Carlos Arce:
Thanks, Chris. So, Sol, we know obviously we started this work interacting before a pandemic, right. and we were using best practices and understanding how the brain works. Now learning occurs and optimizes engagement so that when you have group or an individual work, you get the most out of that experience. So we were pretty acutely focused on that already. It was a skill set that we had honed and developed over a number of years. And I would say I even got a chance to be a practitioner of that in my world. As the chief warrant officer and health care system, we were using methodologies. Sometimes people refer to them as liberating structures that are really about optimizing the time and energy of the people when they do gather. So when we were starting to consider the challenges of dealing with people who were distributed geographically or just might be distributed because of their office space, they’re different buildings or their particular practice as a difference has a different schedule. We were already having to come up with ways to make it easy for people to just kind of join a meeting and to be able to go in and out of their clinical practice. And then we got a chance to hone that work and get it tighter and tighter. And then unfortunately, we bumped into Pandemic. And fortunately for us, we were able to really create a very engaging and dynamic applications of technology. So much so that when we create those experiences for the folks we’re working with, they tend to pass our name on to people within their organization saying, hey, you can tell us what you’re doing in those meetings because everybody else says you’ve got the most engaging applications of this technology. And how could how could we use this in other areas and other spaces? So, yeah, we want to optimize the capacity to allow people to join individually with a coaching session using technology, but also in these group sessions in a way that are highly engaging. Get a chance for people to meet one on one, just like they would in a group. We’re trying to emulate all those things that create community, that create those collegiality support networks where people start to realize that they’re not in this alone, that what they were experiencing that felt like daunting was not is not necessarily just their experience, but some of their colleagues are. And to do that, you have we had to leverage the technology in a way that would really optimize that experience.
Saul Marquez:
That’s great, guys. Thank you for that. And I think in these times, the virtual component is key. And we’re we’re in this reality today where this virtual component is going from necessary to wait a minute, this actually works better meeting people where they are from, from a care delivery perspective, but also from a coaching and an organizational development perspective. We’re all very busy. And I think, you know, the the silver lining of this covid epidemic is that it’s forcing us to use virtual more. You guys have obviously adapted it and it’s going well. You guys are ahead of the game. But, you know, for for for those of you listening, you know, elation does their work virtually. So if you’re finding the morale or the mindset or the burnout level to be high among your physicians, nurses, health care providers, and this is a good opportunity for you to check out an organization that’s doing some incredible work with some with some big names in the in the industry today. So totally direst at this point. And there there stuff works. So let’s talk about that. And you guys don’t have to mention names of organizations or people here, but know give us an example of some of the results you’ve been able to create for for some of the provider organizations you’ve helped.
Chris Dimock:
Also, chime in here, if I may. You know, we had one position that I was chatting with shortly after we ran through a cohort, and her comment to me was when she started, she had a D minus relationship with her physician colleague who co ran the department with her. And she said at the end of the 90 day engagement, her relationship was an eight minus.
Saul Marquez:
Nice.
Chris Dimock:
She admitted that she had been kind of struggling with frustration and depression and. And yet she was also very aware that as she filled out the form for admitting privileges every year, there was a little checkbox that said, have you sought or used UAP services or counseling services for the last twelve months? And she said that had a very chilling effect on her because she just didn’t know what happened, if you basically use those kind of services. And she said it was wonderful for her because she said with integrity, I could not do that because I had a coaching experience. And that coaching experience was transformational for me. And I feel like I’m very much in control of my destiny. And I she’s gone on to do some wonderful things on a statewide basis. So it was a really heartwarming story.
Saul Marquez:
That’s really great. And just taking it. So so going from a B minus and A minus, what did that what did that translate to, Chris like? You know, for her and maybe for the organization.
Chris Dimock:
Yeah, well, in her case, it was was a D minus.
Saul Marquez:
Oh D minus. Oh, wow. OK.
Chris Dimock:
Yeah. Yep. That was a..
Saul Marquez:
I’m thinking one letter big, right.. OK. And three letters here.
Chris Dimock:
What was needed was a fundamentally dysfunctional relationship and a very critical development within the hospital. And their comment is that they’ve now had very constructive engagement and actually proactively designing things that they want to do to help improve the quality of services they provide. And it’s I mean, it’s just hard to do that if you’re personally feeling, you know, not at your best and you’re going into work every day with a colleague you don’t want to be with. I mean, you can just imagine the kind of outcomes get out scenario versus being, you know, engaged and.
Saul Marquez:
Yeah. And I think we’ve all worked with somebody we don’t like at some point or another and or that we just don’t get along with Right. we try to like, but we can’t get along with. And and it’s stressful. And you don’t want to be there and then your work suffers.
Chris Dimock:
Yeah, it does. It does, and I mean, she obviously understood that she doesn’t have control over her external circumstances, but what she does have control over is how she thinks about it. And that was sort of a transformational change for her, shifting her thinking about her relationship with her colleague and her relationship with our patients. So it was a sort of heart warming.
Saul Marquez:
For sure. And we you know, so as you know, as health care leaders and specifically, you know, providers, Right. physicians, you start to have this expectation of yourself. And society expects that you have the answers and that has psychological effects on you. And you throw on responsibilities with H.R. and then you throw in covid. It’s a it’s a it’s a recipe for for stress, depression and disaster. Can you guys talk about what you’re doing with Covid and some of the work you’re doing around that to help out provide organizations?
Carlos Arce:
Yes I can visit a little bit about this. Chris made a reference earlier to the idea of using the virtual technology to connect folks Right. you have a big, daunting problem like this. One of the biggest known unknowns of the biggest threats is uncertainty. What do I do? How do I do it? So we’ve been able to be part of conversations with not only local providers, but federal sources to connect people, to be able to create collaborative conversations about what makes sense and how to progress and building that sense of collegiality. And sometimes it’s bridging folks and connecting people in a way that they can. Problem solved specifically to an area in issue. So, for instance, in one particular case, we had the opportunity to work with what would be considered a rural state, United States. They’re trying to respond in a constructive way. But at the same time, the some of the directives that they’re having to respond to don’t necessarily feel like they apply. So how do they come up with a quick strategy to make sense of it? And then within their state itself, they had a couple of urban communities that really were concerned in a different way than some of the rural areas were connected. And so we were able to help design and facilitate those discussions in a way that take into account the the learnings that we have been able to achieve, but also to be able to build a sense of community that in truth, it kind of increases people’s capacity to innovate and to problem solve. All right. Because now they’re connecting with folks and are learning from each other and they’re be able to look at what that the bigger picture of that that mode. Chris, I know you’re going about to say something. I just, you know. Any other thoughts on those spaces? But we have been trying to up to our clients are in the middle of these things. And I don’t know to what extent we want to put them on the spot. But I know that their ability to juggle multiple things and then maintain their focus on their people. Right. Because they’re trying to take care of the outside world, prepare for their patient load. What’s it going to look like? We have to shut down things. And as a result, our revenue streams have been really been been just undercut. How do we do all those things? And at the same time, turn to our co-workers on a daily basis and say it’s gonna be OK?
Chris Dimock:
And that’s actually cause Carlos alluded to I mean, having good information is even more critical now than ever before. And so we’ve used this period in which a lot of our clients are refocused on being prepared to really help design an assessment tool unique to the health care industry. So Carlos has been working with a psychometric specialist that works with us on the design of a tool to look at wellbeing for physicians, other medical providers and administrators with a particular eye to the stress and anxiety that returning to work in a new covered environment could cause so that people in leadership positions in health care can get a snapshot of how their organizational well-being is at a given point in time. And we sort of fondly refer to it as a PNL of being, because if you use this tool for your entire organization to get kind of a snapshot of what departments are stressed, which departments are doing better, and also a little bit of a prescriptive recommendation around what you can do about that. And so we’re finishing that tool up, working on the validation component of it. And we’ll have that ready in just a few weeks.
Saul Marquez:
That’s exciting. And so, you know, as you guys built the business, I mean, you’ve done an incredible job, right? You’ve you’ve put together a great team. You’ve got a suite of solutions, a proven process that ties to two and complements the existing efforts around safety and quality fruit for these organizations. What’s been a setback? You know, what has happened that you’ve learned from that’s made you guys better today?
Carlos Arce:
I think I think I can acknowledge that it’s yeoman’s work. I sometimes say there’s rigour to shifting your organizational culture. There’s there’s a it’s a it’s a real problem. This is a deeply rooted challenge. It just didn’t happen overnight. We just did not listen. Oh, we should turn that on. Oh, we shouldn’t ever use that EMR. If you did just not use any EMR, we never would create burnout. That’s not what’s happening here. Right. what’s happening is we already had an environment where stress and a lot of the challenges that people experienced that could lead to burnout were were Right. they were there. But if you created enough balance and you created enough of the reward piece, then guess what? You can make a tough situation rewarding and and really fruitful and blessed profession to be part of what is happening over time is that that shifted. And for a lot of different reasons and without pointing fingers, the reality is it’s a complex issue. It is a complex, dynamic, complex challenge that we have. And so to address that, it’s it’s going to require some work. It’s going to require some serious people, some people who are humble enough to be able to roll up their sleeves and say, hey, we acknowledge that we’re contributing this in some way. And to me, that’s the that’s the AHA Right.. It’s the same discovery I made 50, 20 years ago when I was I was working on that whole area of continuous improvement, lean and, you know, reducing waste and unnecessary variation. You know, it’s it’s at my it’s at my core. But I also know that it’s it’s not for the faint of heart. And so that it becomes sexy on the outside. Think people all want to talk about, yeah, we want to build resilience. We want to do these things. Yes, yes. Yes. But when you really sit down and you say, hey, are you are you prepared to do the work? Do the heavy lifting, that becomes the aha moment. Right. Because the truth is, is that there are a lot of well intended solutions out there that still require folks to own them internally. You know, any good executive coach knows that the worst thing that could ever happen is that you want it more than your coach. Right. Because now you’re forcing people to try to do something that that they have not yet seen. And so that to me is my personal highs, the importance of having those conversations early on, acknowledging what you’re trying to get into and making sure you’ve built some partnerships with the the hosts that are inviting you into their organization.
Chris Dimock:
Now, and I would just add that. The hallmark of a bunch of our work is that we have worked to take the well-established neuroscience to cure rate, a methodology to help people fundamentally shift mindsets. So how do you change habits? How do you change your view of yourself and your relationship to the rest of the world? I would say, you know, we have years trying to apply the best research we can find to build out this methodology. And that is one of those cases where you are very humbled by the realization that, you know, 70 or 80 what you think doesn’t work the way you thought it should. And so it really has been a long and arduous process, sort of distilled down the elements of how you help people change their thinking. Now, the upside, of course, is that because we do pre and post assessments, we are very diligent about looking at the impact of our work. And we do follow up interviews to make sure that the impact of the sustainable impact. So we’ve tried to turn the curse of the trial and error into a blessing, which is a well curated type process that we can deliver effectively.
Saul Marquez:
Love it now. This is great stuff, guys. And and every every successful business goes through those challenges. And then they figure out a way to to make differentiators out of that. And you guys certainly have what what are you guys most excited about today?
Chris Dimock:
Well, I think, you know, for me, it is the upcoming assessment tool, this idea that we can actually fundamentally present new information to leaders in organizations where they can have this kind of snapshot of the well-being of by department, obviously, the data identified. But, you know, to actually look at your organization and say, you know, there’s an unusual amount of stress in the cardiology department, maybe we should go look at what’s going on in there to see if there’s something that we can do in a constructive manner. I think that’s the kind of data that that we always hoped we could get but never really had access to. And I think that this assessment tool we’re working on will actually provide that. And so we’re very excited to partner with a handful of health care organizations that are interested in that.
Saul Marquez:
Is there an invitation for others if they’re listening and curious to join?
Chris Dimock:
There absolutely is. Yes, because, you know, obviously we are staying true to statistically significant data. And so the larger the sample size, the better. And so we are looking for organizations that would like to explore this idea of how to turn insights into organization wide well-being, into, you know, impacts on the culture and operations of the organization that actually make it a healthier place to work.
Saul Marquez:
So, folks, if you’re curious about that and wondering how this this can help you and your organization, I will. Well, we’ll provide a place for you to contact Chris and Carlos to learn more. So so really, I guess, why don’t we do that? I mean, you guys, what where can they where can they reach out to you guys to tell her more about that, but also more about your company.
Chris Dimock:
The company’s Web site is elation.com. And we obviously love the work that we do, but are very interested in talking to the people in health care that would like to explore the idea of these solutions. Either the assessment tool or position informed organization resilience or this mindset based coaching methodology that we’ve developed. Carlos also does a wonderful job with strategic planning and workshops. And so we’ve got a pretty broad cross-section of services we offer. And as I say, we are sort of a boutique company and that we craft solutions unique to each of our clients. And so we’re very proud of that personal attention that we can have it.
Saul Marquez:
And so so, folks, there you have it. Elation.com to learn more and leave us with the closing thought, guys, where should we be thinking about what should we be doing as a result of, you know, the work that you guys are up to and what you’ve brought to our focus?
Carlos Arce:
Yeah, I would just offer that a lot of the solutions to this work lie within each of us. Which is why we’ve all become more reflective. You know, we’ve been spending more time. We’re seeing increases globally around people exercising on their own, finding a place where they can go for a walk. I mean, there are some pretty powerful capacity, neurologically physically that that impacts us. And so now I’m just invite people to make sure that you’re tapping into the resources around you. You’re looking for ways to be able to build collegiality and support that social connection. While we’re social, isolating is important. And in the health care space, too. Don’t do not underestimate the the challenge of trying to be the role models that every one of your health care organization wants to be in your communities. And at the same time, be the kind of employer that’s able to create as kind of a work life balance and a health culture that can thrive and adapt to to a challenge like this, but to future challenges.
Saul Marquez:
That’s a great that’s a great call. Chris, go ahead. You had another one.
Chris Dimock:
I would echo that point, too, which is, you know, there is sort of a famous gap between administration and clinical providers, but lot of health care systems. And as difficult as it sometimes feels, the only real sustainable long term solution there is helping to bridge that gap and bring people together. And the common are those of improve patient outcomes and operating a physically healthy health care system. And so, you know, it’s a daunting task. But it’s one that we’ve got experience in helping people bridge and the results that we’ve gotten. I speak for themselves. We love talking about.
Saul Marquez:
This is great, guys. And and folks, you know where to go. outcomesrocket.health in the search bar type in Elation. And you’ll find a full transcript of our discussion with Carlos and Chris, as well as show notes, links to all the resources we provided and also a white paper that they did. That will include their a project to enhance physician resilience and mitigate the risk of burnout. That just kind of gives you a sneak peek at the quality and research data driven work that they do and why they get results. I was blown away by by their method. And and so I wanted to post that for you guys to learn more about how they do what they do there. But, yeah, I just want to thank you guys so much for for the work that you’re doing, number one, but also for for taking the time to share it with with the community here with us. Chris and Carlos, big thanks from all of us.
Chris Dimock:
Thank you very much.
Sonix uses cutting-edge artificial intelligence to convert your mp3 files to text.
Sonix takes transcription to a whole new level. Sonix converts audio to text in minutes, not hours. More computing power makes audio-to-text faster and more efficient. Do you have a podcast? Here’s how to automatically transcribe your podcasts with Sonix. Get the most out of your audio content with Sonix. Lawyers need to transcribe their interviews, phone calls, and video recordings. Most choose Sonix as their speech-to-text technology. Sonix has the world’s best audio transcription platform with features focused on collaboration. Are you a radio station? Better transcribe your radio shows with Sonix.
Sonix is the best online audio transcription software in 2020—it’s fast, easy, and affordable.
If you are looking for a great way to convert your audio to text, try Sonix today.
Things You’ll Learn:
Resource:

