Pain management requires reforms to tackle the opioid crisis and obesity.
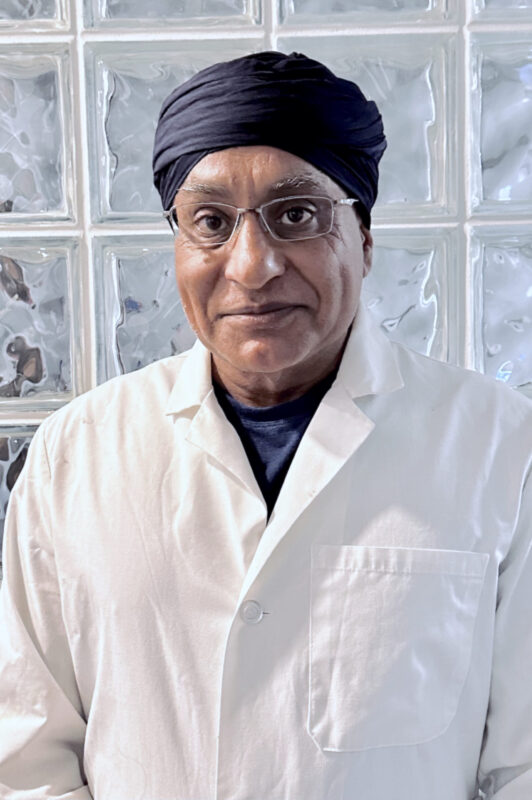
In this second part of our conversation, Gurpreet Padda, a seasoned pain management specialist, discusses the overprescription issue driven by pharmaceutical misinformation and the role of pain management in reducing opioid use through interventions. Dr. Padda highlights the link between obesity and chronic pain, and criticizes dietary guidelines heavily focused on carbohydrates and vegetable oils for contributing to inflammation and insulin resistance. He explains pharmaceutical companies’ significant involvement in the opioid crisis, along with the escalating fentanyl problem, and how countering pharmaceutical influence and embracing AI technology could play a pivotal role in reshaping healthcare. Dr. Padda believes physicians should challenge norms, prioritize patient education, and advocate for systemic changes to tackle chronic pain and disease.
Listen to what Dr. Padda thinks are necessary systemic changes to tackle the opioid crisis and promote better health outcomes!
Dr. Gurpreet Padda is an esteemed physician with over 25 years of experience specializing in pain management in Saint Louis, MO. He graduated from the George Washington University School of Medicine and Health Sciences in 1992 and is affiliated with SSM Health Saint Louis University Hospital.
His holistic perspective has led him to explore the intricate connections between chronic pain, metabolic health, addiction, and social determinants of health. This perspective has driven his innovative strategies in pain management, where he strives to address the root causes and provide comprehensive solutions.
Download the “Chalk Talk Jim_Dr. Gurpreet Padda Part 2 audio file directly.
Chalk Talk Jim_Dr. Gurpreet Padda Part 2: this mp3 audio file was automatically transcribed by Sonix with the best speech-to-text algorithms. This transcript may contain errors.
Jim Jordan:
Welcome to the Chalk Talk Jim Podcast, where we explore insights into healthcare that help uncover new opportunities for growth and success. I'm your host, Jim Jordan.
Jim Jordan:
Welcome back to part two of my conversation with Dr. Gurpreet Padda. In part one, we discussed the origins of the opioid crisis and the innovative approaches to pain management that considered metabolic health. We're going to pick up where we left off, exploring opportunities like changing dietary guidelines and better-utilizing technology to improve healthcare outcomes. Dr. Padda, it seems like the opioid crisis had caused the pendulum to swing in the opposite direction in terms of prescribing. Has this led to a decline in the number of pain management centers, and was overprescription mainly an issue stemming from pain management centers originally, or was it a primary care issue?
Dr. Gurpreet Padda:
There's probably, similar, went down. There's not a huge number of centers, There's a demand, but there's not a number of centers. And if you look at the primary driver for usage, you're not going to see, the primary prescriber of high-dose opiate is typically the primary care, and we see that all the time. We get patients in, and they're on 200mg morphine equivalent per day. Our job is to wean them down. People think historically, no, it's the pain management center that's going to put them on the opiate. It's usually the patient comes in on opiate, and then your job is to use interventional procedures to lower them down. Now, that's separate than what a pill mill is. A pill mill is some center that someone has set up, it's usually not even a physician. Usually, it's an organized crime ring, and they're using it to distribute narcotics. There were a bunch of them down in Florida for years when people would traffic from Florida up to the rest of the United States, and they would pick up their narcotics down there because the regulations were loose. But those regulations tightened maybe six years ago, and so a lot of those pill mills simply disappeared. There's still bad actors, obviously, because people will be people, and they will do stupid things, and there's always an incentive to skirt the law. But most people that are doing interventional, their main thrust of pain treatment is to use the least amount of narcotic and use procedures to turn off pathways and then do something else. So the thing is that if I give you a narcotic and I give you a high-dose narcotic, the first thing that happens is, one, I activate your dopamine. But more importantly, within a few days, you become tolerant to it, and even more importantly than that, you stop producing endorphins. And so when you stop producing your endogenous endorphins, and I take away that high-dose endorphin that I've produced, given to you systemically from the outside, the exogenous stimulant or exogenous endorphin, you start to go into withdrawal not just from the lack of opiate, but you generally feel like shit because you can't produce enough endorphin and you really hurt. And so, the goal of a pain management location is to use the least amount of medication so the patient still senses the pain, but you can turn it off through other modalities, and sensing the pain allows the patient to continue to produce some of their own endorphin. Your goal is not to get their pain to zero. If you get their pain to zero, you've done the wrong thing. If you get their pain to 1 or 2, you've done the wrong thing. You want them to have daily production of endorphins. You want the body to continue to produce endorphins, and you use these short-acting additional adjuvants that we're going to provide exogenously to just take the edge off.
Jim Jordan:
In preparing for this interview, I did some research on you, and it struck me that losing weight and being mobile seemed to be one of the things that your many patients were thankful for. Is this part of your strategy?
Dr. Gurpreet Padda:
Of extra excessive load that you're carrying, you're putting 240 pounds on the spine. These patients are coming in 100 pounds overweight … that they're burying on their spine. That's like carrying a small baby elephant on your back. So the axial load is significant, but even more significant, when you have estrogenic obesity, you're producing inflammatory cytokines. So here's how this works. So it's real, it becomes, because most of your audience is physician, so they're going to grab this immediately. So if I give you a carbohydrate load orally or systemically IV, you're going to produce insulin. If you produce insulin, takes the circulating glucose, and shoves it, it lowers systemic glucose. It doesn't do anything fancy, but grab circulating glucose and shoves it into your cells. And if your cells are already full, if you haven't depleted your glycogen reserves, it goes to fat. And as you get more visceral genic fat, there's a hormone that's produced by fat called leptin. Leptin tells your brain you're full. When you get more and more overweight, you become leptin resistant. So not only are you insulin resistant, your leptin resistant. So what's the big deal there? The big deal is leptin is the most potent inflammatory cytokine we have, and high systemic leptin causes you to hurt everywhere. And so it's a necessary thing for you to be hyper-inflammatory. And so, hyperleptinemia is closely associated with this. And that's, what we have to do is we have to unwind all that, make leptin sensitive again, drop your leptin levels, bring your estrogenic fat down, and then start mobilizing your joints so you get fluid in, and so we spend a lot of time.
Jim Jordan:
Our list has included a diverse group of people from all over the healthcare industry, from physicians to insurance providers, nurses, and other stakeholders. With this in mind, could you give us a sense of what proportion of overall pain treatment is carried out by these pain management centers? And also, could you explain how the referral process works? Are pain centers typically where patients end up when primary care physicians are unsure how to handle the onset of a patient's pain cycle, or are there other circumstances that lead to these referrals?
Dr. Gurpreet Padda:
Yeah, so our average patient has had pain for 1 to 3 years minimum. Our average patient has been tried by their primary care, tried by Orthopedics. The average patients coming in, if they're coming in through their orthopedic, they're usually on 60 to 80mg morphine equivalent. If they're coming through their primary care, they're on 160 to 200-milligram morphine equivalent. The average patient, not average, 99% of the patients plus have severe systemic metabolic inflammation, which means elevated hs-CRP, insulin resistance, high …, high LPIR, high LDL-P. So all of these biomarkers that we use to identify systemic metabolic inflammation.
Jim Jordan:
So for our audience, that wouldn't be a traditional thing that they would be thinking about when dealing with pain, correct?
Dr. Gurpreet Padda:
In this niche field, and so we get patients that have been kicked out because, I've given you the meds, you're not getting better. I've done the surgery, you're not getting better. Yeah, they're not going to get better. They have something else, they have systemic issues. And so that's the patient that we see. We get patients that come in 450 pounds, and a year and a half later, they've lost 150 to 200 pounds, and we get them off out of their wheelchair, and we get them walking.
Jim Jordan:
When you look at diabetes, and there's some pretty solid protocols on when we get folks over to an endocrinologist, and we have training programs that have reimbursement codes for all that, as I'm listening to you, I wonder, and I'm guessing that we do not have such codes for pain management.
Dr. Gurpreet Padda:
No, and for example, we have to, when I do this, I take these diabetic patients, and we make them nondiabetic. We wean them off their insulin, we deprescribe. That's how I spend most of my day, trying to deprescribe because they become hypertensive; they become hypoglycemic if you leave them on their meds, if you leave them on their high-dose insulin, so we have to taper down that insulin. And so that's why I had to get additional training, the Society of Metabolic Health and Nutrition, National Nutrition Association, and a whole host of other people, low carb USA, and low carb Denver, and all these other groups. I had to get significant additional training to understand how to deprescribe, because as soon as I can get their weight down a little bit and as soon as I reduce their glucose, I get them off their insulin. That's a savings, if you take somebody off of insulin, you're saving just on pharmaceutical costs $1,400 a month on average. That's $13,000, $14,000, $15,000 a year of pharmaceutical costs. And usually, as soon as you reduce their insulin and you get rid of their sugars, their blood pressure goes to normal because sugar is the primary driver, it's not salt. See, the thing is that people assume that it's excessive salt consumption, that's the issue, it's not. It's the excessive glucose consumption which affects the pre-renal, which affects pre-renally, and it's the insulin level that the proximal tubule that causes the salt retention. But if you get rid of the glucose, you actually …, and the bigger problem is giving these people enough salt because they actually become hypovolemic very quickly, and they lose so much salt that they'll go into atrial fib, and they become hyponatremic. So you have to, that's what I spend my time doing is deprescribing them and getting them off of these drugs, and it's pretty robust. You can take, I take patients that have been diabetic for 10, 20 years who are type two diabetic, not type one, but type two, and you can radically change them so that within 2 to 3 weeks, they're almost all off of all of their insulin, and it's a dramatic shift.
Jim Jordan:
As we reflect on the opioid crisis and its ongoing impact, particularly in relation to the role of pharmaceuticals, I'm curious about the specific challenges that your organization is now confronting. Are there new issues that have arisen as a result of this crisis, or perhaps any improvements or silver linings that you've noticed? Additionally, I think it would be beneficial to understand more about the origins of the opioid crisis. You've previously mentioned the role of the pharmaceutical companies. Could you elaborate further on their actions and the overall impact they had in precipitating this crisis?
Dr. Gurpreet Padda:
I think the issue is the misunderstanding. So let's, we're in a different situation. Let's talk about why we got into the opiate crisis in the first place. It was pharmaceutical companies that got us into the opiate crisis. They hired some attractive, very forthright representatives that went into physicians' offices, gave them studies that were fabricated, that showed that OxyContin was a 12-hour drug and it was low diversion risk. And Purdue knew that was wrong, they basically made up the studies.
Jim Jordan:
And anyone that's listening, there's a wonderful Netflix series, which I'm sure is not 1,000% fact-based, but it does give a shocking overview of that story and sadly also casts a shadow on legitimate pharmaceutical companies.
Dr. Gurpreet Padda:
Yeah, so we had these pharmaceutical companies that were pushing a treatment modality and funding a lot of speeches for people to prescribe more. It's basically the origin of how physicians started, actually, because physicians, if pharmaceutical companies needed salespeople and they funded the first medical schools because they needed highly educated people to convince the public to use their drugs, and so physicians were, is how that started. Physicians are, they're an arm of the pharmaceutical company, in essence, because they're the ones that do the final signature that allows the pharmaceutical company to dispense and distribute their medication. So the opioid crisis starts when these pharmaceutical companies want to sell a large amount of very cheap drug and put some proprietary technology on it and use that to harvest the money out of the healthcare system. They inadvertently, they get a bunch of people hooked, and the people that are receiving these medications realize that you can snort the stuff, and there's no deterrent from doing that, so they get a massive high off of that. But that was part one. Part two is different, though. Part two is our current opiate crisis. So the prescriptions that are being written are way, way low. The reason why there were so much prescriptions written in the beginning is that if the only tool in your tool belt is writing a prescription, and you can't do anything to treat the pain, and you don't recognize the other factors, then you're going to write a prescription as a primary care because you're going to go, I'm just going to write this prescription, you're going to get better, because I've been told that OxyContin is not addictive. They've been told that, and they've been pointed out these studies that this is a 12-hour drug, and it's fine, it's safe, nobody gets addicted. It's not true, that's how it starts. Where we are now is different, though. We're fighting the second Opium War. The first Opium War was the British tried to open up the ports in China, and they got people hooked on heroin, and they forced the ports open because the Chinese wouldn't let the Brits trade, and so they got locals addicted on opium that they had harvested out of Afghanistan, Pakistan, and India. Well, we're fighting the second Opium War, what's happened is that China is producing the reagents for fentanyl, which is a and other things, and they're shipping it into Mexico, and the Mexican drug gangs are shipping it into the United States as a finished product and selling it. And the second drug war is dangerous because the thing is, unfortunately, the people creating these, taking the reagents, and creating the finished product are not very good at quality control. And so you might be getting 2000 micrograms of fentanyl, you might be getting 20,000 micrograms of fentanyl, or you might be getting 200 micrograms of fentanyl in that dose … There was a recent seizure in Southern California where somebody brought over a small amount of fentanyl. It was of such high quality that it would kill about 30 million people. It's a weapon of mass destruction. And so if you aerosolize that, you could take out a city, and so these are the issues that we're dealing with. We're dealing with the second opium war. And it's, underneath this is, it's a way to, if I was looking at it from a political standpoint, it's a great way to destabilize the country. It's a terrible thing. And there's still a confusion when people think about narcotics, they think, they don't understand the difference between illicit and elicit. We use fentanyl all the time in anesthesia to assist during cardiac operations. For a pediatric heart-liver lung transplant, you use fentanyl. For adult cardiac, you use fentanyl. But we know how many micrograms there are per milliliter, and we know what dose we're giving to the patient, and it's under controlled ventilated environment. The fentanyl you're getting on the street, which now they're mixing into weed, they're mixing into cocaine, they're mixing into methamphetamine is a problem. And now they've added all kinds of other things like xylazine into it. And Xylazine is an animal tranquilizer that cannot be reversed with Narcan. So now the, if you do find somebody who's overdosing on fentanyl and you give them Narcan, it won't work because there's 90% of the samples of fentanyl have Xylazine, and it's unregulated, and so the dose of xylazine is extraordinary. And so you may not be able to reverse them at all, even if you find them.
Jim Jordan:
So for your practice, the legitimate patients with pain issues, is there a different challenge they have in getting help today than they did ten years ago?
Dr. Gurpreet Padda:
Oh, yeah, absolutely. So it's all incentive-based, and the pendulum always swings. Walgreens and CVS were considered co-conspirators to this pharmaceutical overuse, and so they themselves got punished. And so they have incentivized their pharmacy representatives, the pharmacists, to not fill medications because there's this misperception, oh, this patient's getting three Percocet a day, he must be a drug addict, and I'm going to not fill because if I can show that I didn't fill a medication, it makes me look better, and I've been incentivized, received accolades from my compliance division. So now patients face this, they become pariahs in the pharmaceutical world.
Jim Jordan:
I think the word pariah is really interesting. I've had family members and specifically my father who faced a tough situation at the height of the opioid crisis. He had undergone severe lung reduction surgery, and they literally sent him home with the single pain pill and a prescription. And his partner, who didn't have his last name, was denied the medication when she tried to pick it up, leaving him in significant pain. And fortunately, I just happened to be visiting, and I'm a junior, and so I was able to retrieve his medication for him, but it just underscores how the pendulum can swing to the extremes in these situations. Similarly, I spoke to someone who was frustrated by the requirements for their ADHD medication. Every month, they need a physician's prescription from their doctor, which they need to physically take to the pharmacy. They can't get anything electronic with this. And the issue is, they humorously noted that if they could remember all the details, they probably wouldn't have needed the medication in the first place. So considering these swings, what challenges are you currently facing in running your practice that you didn't encounter before the opioid crisis?
Dr. Gurpreet Padda:
Yeah, so I think that, and it's not just us, it's not just me. It's the, I think the number one challenge that physicians are going to have is that we've got an initiative in the United States that the public health officials, the masters in public health officials, are really driving healthcare, and they're using it using data analytics, and they fundamentally misunderstand and mischaracterize what's actually going on. So you've got all of these review agencies that look at healthcare, and they're basing it purely off of looking at statistics, and they go, this guy does this and this, and he's an outlier, therefore he's wrong. And this guy does this and this, and he's an outlier, and he's wrong or she's wrong. And so they look for outliers, and they're not looking at clinical outcome, they're just looking for outliers because statistically, that's easy to identify and outcome is hard to identify. And if you looked at statistical normality, only 7% of the US population is healthy. And so if you want to maintain not being an outlier, you would just continue to maintain that 93% of unhealth in the United States. So the problem is that from a statistical standpoint, people, the analytics done at Medicare are looking to quelch outliers, which prevents getting better because we've gone down the wrong track. 93% is sick, and if we want to prevent outliers, we're going to prevent that 3% from ever getting better.
Jim Jordan:
So is it just more money? What does it take to make this better?
Dr. Gurpreet Padda:
So it doesn't take much money, and that's the interesting thing here. We talk about a physician shortage. We don't really have a physician shortage, we have a disease excess, and we have plenty of physicians if we don't have disease excess. So it's not like we need more physicians if we reduce our disease burden, which can be done through dietary change. So what, I think that we need to take one step back and ask ourselves how we got here and how is it that we're here. And I think that, if you get that insight, you realize what happened, and that's what I would fix. So here's the step back. The number one purveyor of sugar-sweetened beverages, the number one consumer of it is Walmart, because that's where most of the subsidy dollars and that's where a lot of food stamps go to. So take a step back from that. How did we end up with food stamps? We ended up with food stamps because, before World War One, we had an issue, between World War One and around that time, we had the issue of a dust bowl down in the desert southwest where people were dying of malnutrition. The United States was afraid that if we got attacked, we wouldn't have enough of a population to defend, and the number one reason why people couldn't be enrolled in the armed forces was malnutrition, they were dying. So they decided to create a subsidy. They took food from the Northeast, process it, and sent it down to the Southwest for civil defense. The big Agra got addicted to these subsidies that they were getting to produce this hyper-processed food. And at the same time, we started using more and more vegetable oil, which happens to be hyper-addictive to humans. It produces compounds that affect human biology, and it's very similar to Anandamide. At the same time, we had the dietary guidelines kicked in in 1971. We had increased use of vegetable oil, which Ancel Keys said was heart healthy and a big food and big agriculture paid off all kinds of societies, and we ended up basically high vegetable oil, high carbohydrate dietary guidelines, which are followed by almost everybody, including the armed forces. So here we are with a population that's getting fatter and fatter, more and more insulin resistant, so now there's only 7% of us that are healthy. So now we've unwound this, so how do we reverse this thing? First thing I tell my patients is eat like your grandmother or your great-grandmother. Quit eating all this stuff, the type of processed. I think we need to look at our incentives. The biggest incentive that we need to fix right away is how we're distributing food subsidies. And one of the issues that I've got is we're about to go to universal basic income. And when we get UBI, we're going to have a problem because people are going to be incentivized to get hyper-processed food that is hyper, hyper-palatable.
Jim Jordan:
Explain UBI, for our audience.
Dr. Gurpreet Padda:
Universal basic income, we've been experimenting with it on and off, and COVID really allowed a mass experimentation. The problem is that when you give people money, universal basic income, certainly they don't starve to death, but they spend it as efficiently as they can to get the most amount of carbohydrate and satiety and feeling of generalized well-being, which is dopaminergic. And the food companies know this, there's a book called The Dorito Effect that talks about the food science that goes behind producing a bag of Doritos. In that Dorito bag, it's not just one Dorito. What it is, a variety of different Doritos that have different flavor profiles and hotness so that your sensory-specific satiety on your tongue never gets tired so you eat the whole bag; because if it was just one flavor and one level of hotness, you would stop after about 5 or 10 Doritos. But because you keep chomping and you get a different flavor profile, it confuses your tongue, and you never get the sensory-specific satiety. It's like sitting down and eating a steak, and I give you 4 pounds of steak, you get tired of eating after a couple bites, and you go, I can't eat the rest of this, but all of a sudden, I present you with dessert. You go, hey, I like dessert too, and you have a dessert stomach, it sends through specific satiety, so the big food companies have engineered our food to do that. And same thing with fructose, high-fructose corn syrup. They figured out the dopaminergic action of fructose in the brain and actually engineered the high fructose corn syrup to be hyper, high-fructose corn syrup. Should be 55% fructose, but they produce fructose at 60 to 65% level in this sugar-sweetened beverage to make it more addictive. So 15 minutes later, you … again for another sugar-sweetened beverage. So I would go back, and I'd say, look, let's get rid of food subsidies for hyper-processed food. Let's not let you use food subsidies for hyper-processed food. Instantaneously, the big agricultural companies would all immediately change their production, instantaneously. If you said that there's no, we're not going to allow you to use this UBI or food stamp to get hyper-processed food, you have to buy real food, and you can't buy stuff from, that you can tear open in a bag and pop in your mouth without heating or any manipulation, that makes an immediate change, and it would immediately affect the outcome. If we legitimately looked at our dietary guidelines and said maybe vegetable oil is not that healthy for us, which we know it's not, maybe change away from vegetable oil, maybe change away from grains, maybe change away from carbohydrates. If we change those dietary guidelines, if I had unlimited resources, I would instantaneously change the food system first, and everything else would fall in place.
Jim Jordan:
It's true. I think if we could solve for quality of food, genetic issues, and environmental issues, we'd probably actually solve all. … lesson you've learned in your healthcare journey thus far?
Dr. Gurpreet Padda:
What I've learned the most? When you try to make a change, and you try to make a population-level change, it can smack you in the face because the healthcare system doesn't want to change by itself, and so you will run afoul of existing dogma that you don't expect. And you say, this is the right answer, though you can't just see these studies? This is the right answer. But no, the dogma doesn't want you to change. See, good science doesn't get better because we have studies; good science gets better because our bad scientists die, and those people finally give up, and they go to their funeral or their grave, and then, all of a sudden, we jump science. And we've been stuck in a dogmatic approach for a lot of stuff. And so it's going to take time. It will happen eventually, we will eventually get there, but it will take time. And so one of the things is that people that deal with this area, which there's not too many people that deal with this, but there's still probably 5,000 to 10,000 physicians in the United States that have come to this realization the same way I'm headed, is that we're going to figure it out. But there is an overarching conspiracy that you're fighting against and not conspiracy-like secret, this is evident. It's just conspiring together to create an effect that you don't. It's unintended consequences in a complex adaptive system with a butterfly effect, that's what we're dealing with. It's this whole thing of like, breakfast is the best meal of the day. Everybody knows that. No, it's not. That's just a marketing slogan by General Mills from the 1940s. Why did they have that marketing slogan? They did that because it encouraged you to eat healthy breakfast. Yeah, actually, what it did was it encouraged you to eat a healthy breakfast of cereal, and then you got hungry two hours later, and you ate more, then you got hungry two hours later, and you ate more, and so you ended up having three main meals and five snacks in the daytime. But if you skip breakfast, which is supposed to be the healthiest meal of the day with cereal, all of a sudden, you're not having five snacks and three meals a day. So it's this dogma that we have to recognize and call out. A lot of our issues with people claiming that veganism is incredibly healthy, that's built out of Loma Linda, California, it's a Seventh-Day Adventist. … Kellogg is John Harvey Kellogg was a Seventh-Day Adventist. He was the typesetter for the Seventh Day Adventist when he was 7 or 8 years old. And when he ran insane asylums in the Northeast, he wanted to have his male patients quit masturbating. He felt like their testosterone was so high, so he fed them cereal, which then made them overweight, and their testosterone dropped. Then he started popularizing the use of Kellogg's cereal, and that's the origin of how that started. So if you go back in the origin story, all of that information is there. It's not a conspiracy, nobody's hiding it, but it's right there in front of you. And these are the things we have to analyze and get back to. There's no vegetables in vegetable oil, but yet the name is vegetable oil, it makes it sound healthy, but there's no vegetables in vegetable oil. It's hyper-refined seed oil that was considered a biohazard for animals. And for years, it was illegal to give it to animals because it made them sick and diabetic and made their meat taste bad, and that was in the 1800s. We've known that, so that's not new news.
Jim Jordan:
To end on the, I think we've had a pretty good discussion on the threats to the US healthcare system. What do you see as the biggest opportunity for growth from your point today, where's the optimism? Where do you see the, some momentum going?
Dr. Gurpreet Padda:
I'm incredibly optimistic. I think that we can solve this. I think that we have to, we can save a ton of money, and we can solve this, because it's pretty simple, it's not super complicated. We just need to educate, and we need people to get, spend time with our patients to educate them. We need coaches more than we need just pure throwing drugs at them. I'm very, as we become more financially constrained as a country and we spend less money on pharmaceuticals because we can't afford it, this is going to actually happen. And so I'm actually thinking that 5 to 10 years from now, our global health level should get better. And with our ability to integrate technology and our ability to use, our ability to use script and AI so we can talk to these robotic agents, I've trained an AI in how to answer questions for addiction, and I gave it a large learning module, and I went through the thousands of questions that patients ask and trained it. And I don't let it run on its own, but I'm right there, but it knows how to answer these questions because it understands the question through a filtering system of what the patient is asking. I think that is going to the big, be the biggest change in healthcare. We're all connected to each other through these iPhones or through our Android. We all have immediate access to remote therapeutic and remote patient monitoring and our ability for patients to connect to us through a chatbot and get the right answer as long as we have the right protocol.
Jim Jordan:
I agree, in the long run, after we've validated our systems, I think technology and AI have a great potential to improve healthcare through better education and monitoring.
Dr. Gurpreet Padda:
This is the simplest example I can give you, there's a beautiful study that came out, just, it's a, it's actually not formally published yet. I saw the data on it, and it should be out formally published within the next three months, and all they did was they gave patients a CGM monitor. They did nothing but give them a CGM monitor, they were pre-diabetic, they didn't tell them what to do. They didn't tell them how to use it, they just put a CGM monitor on them, and they said, hey, our goal is for you to have the least amount of blood sugar possible at all times, and that was the extent of the education, just look at your numbers. And they didn't give them additional education. All of them dropped 1.5% or greater in hemoglobin A1C within a month and a half, less than 90 days, because there was a feedback loop. They didn't need to know much, all they needed to know was this number. See, we don't need to have prompt engineers as patients. We don't need that. All we need to do is produce topical, particular niche for the patient's disease problem that we've identified. And then the physician needs to be the prompt engineer, and the physician needs to say, look, you have this, and this is how this interacts. And so, I'm going to assign this AI to help you for this. And the AI doesn't get tired and doesn't really get mad that the patient's calling them at 2:00 in the morning.
Jim Jordan:
And what's noteworthy to me in terms of providing input and listening to recommendations is that AI doesn't judge you. You're more likely to ask that question and get the education that you need than being afraid of being embarrassed and asking it to a doctor.
Dr. Gurpreet Padda:
And it has guardrails, it keeps you from falling off the track. And so I think, I'm, I think this is the best thing that can ever happen. I know people are terrified, but I really, genuinely believe that this AI revolution that really started December 15th of 2022, that's when it really started, because I've been playing with AI models for years, and they were filtering. And really, when it got to a wide language array, that really made sense, that was in mid-December, and this thing is learning, and I play with it all the time using contemporary data source and have it search through Google to, through Google Scholar to pull up current relevant information. So I think that it'll have a huge impact, and I think physicians will become prompt engineers that will give the data set for that particular patient, and the patient will then be able to have a confidant, and then the AI will tattle on them when they misbehave.
Jim Jordan:
To that point, our data scientists at Carnegie Mellon University often collaborate with physicians from our local healthcare systems. Some of these studies involve individuals opting in to provide information related to social determinants of health that normally wouldn't be shared due to privacy concerns. And interesting, as you pointed out, people often don't follow through on what they tell their doctors they're doing, and this makes it challenging for physicians to provide effective care. Is there an opportunity here?
Dr. Gurpreet Padda:
As physicians, we have an obligation. We've been given a tremendous opportunity to directly interact with our patients. We should, patients look up to us. I realize that there's a lot of conflict that we can have with patients, I realize that we have conflict with insurance companies, I realize that internally we have conflict and egos with physicians and things like that, but we're in a position that we can really impact a lot. And I tell my patients, and I tell people that I work with, look, realize that health is wealth. If you can make somebody healthy, you can really help, but if you have wealth without health, you're screwed. You're not going to get anywhere. And so, I try to emphasize that as a coach and try to approach that. I think that each physician has an obligation to improve their society around them, and we have to be inquisitive. We cannot get sucked into the paradigm of writing scripts because that's the easiest thing to do and it takes 30 seconds. You really have to, we went to medical school because we were smart, and we didn't go to medical school because we were at the bottom of the class. And so we've got intelligence, and we should use that intelligence in a way that's more than just simply being a sales arm for the pharmaceutical company. And that's one thing I would really hope the physicians would do.
Jim Jordan:
Dr. Padda, this has been an enlightening two-part discussion about the intersections of pain management, metabolic health, and the opportunities to improve our healthcare system overall. Just a reminder, in part one, we covered the opioid crisis and the innovative approaches to treating pain without overreliance on opioids. If you missed that, please go back. In part two here, we explored the systemic changes that could help us address the root causes driving chronic disease like revising dietary guidelines and properly aligning incentives. We also discussed the promising role of technology like AI chatbots in providing low-cost virtual care. I appreciate you taking the time to share your wisdom and insights with our audience. There are clearly many avenues to pursue in order to enact meaningful change in our healthcare and public health systems, and I hope we continue this important dialogue in future episodes. Thank you again, Dr. Padda.
Jim Jordan:
Thanks for tuning in to the Chalk Talk Jim Podcast. For resources, show notes, and ways to get in touch, visit us at ChalkTalkJim.com.
Sonix has many features that you’d love including generate automated summaries powered by AI, collaboration tools, powerful integrations and APIs, transcribe multiple languages, and easily transcribe your Zoom meetings. Try Sonix for free today.

