Necessity is the mother of invention and healthcare is replete with stories of medical discoveries inspired by need. Nurse anesthetist Roxanne McMurray was on a medical mission trip to Lima, Peru, with a team of clinicians and plastic surgeons to fix cleft lip and palates in children. One of her young patients had nearly fully fused lips, making airway management and the delivery of anesthesia almost impossible with the available equipment. Using the limited supplies on hand, Roxanne improvised an airway device that worked well to keep the patient breathing, safe, and comfortable.
That situation could have turned out to be just another amazing medical hack, but Roxanne recognized that the solution that she created in a moment of necessity could fill a much broader gap in anesthesia care back in the U.S. The idea for the McMurray Enhanced Airway (MEA) was born.
The increase in nonoperating room (NORA) and outpatient procedures correlates with the growing use of deep sedation, which keeps patient comfortable but ideally also maintains the patient’s spontaneous breathing. After a patient has been sedated, the upper airway often obstructs because the tongue falls back or pharyngeal tissue relaxes closing off the airway. An obstructed airway increases the risk of hypoxia, which can lead to adverse outcomes including brain damage and death in the most serious cases.
To decrease the risk of airway and respiratory complications, appropriate intervention is needed. Anesthesia providers use oral and nasal airway devices to help maintain breathing and ventilation, but the typical products come with potential challenges. Traditional oropharyngeal airway devices are curved, rigid, and generally made from plastic. Injury to teeth or dental work and bleeding are some of the risks. For many older patients who take aspirin or anticoagulants, inserting a nasal airway may stimulate bleeding that further compromises the airway. As a longtime anesthesia provider, Roxanne knew there had to be a better way.
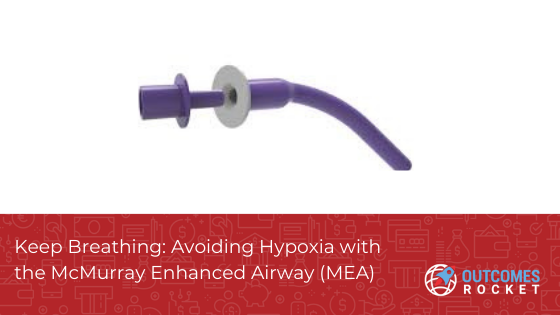
The innovative McMurray Enhanced Airway (MEA) device is soft, flexible, and has a longer and thinner tube compared to traditional oral airway devices. These features make it a better choice to eliminate upper airway obstruction. Plus the MEA has an optional connector to allow intraoral ventilation and forgo difficult mask ventilation. The MEA is safe, easy to use, and quick to place in any patient position.
The MEA is the flagship product of Minneapolis-based McMurray Medical Group, the company co-founded by Roxanne. Roxanne said she developed the MEA to bring a novel and much-needed modern solution to airway management.
“The tools that we have to open the airway are not sufficient because they only reach the back of the tongue,” Roxanne said. “To maintain an open airway, we sometimes need to lift the chin and jaw and hold those positions for the duration of a procedure. That can result in post-operative pain for patients to the point that after their surgeries, they complain more about chin and jaw pain than incision discomfort. Also, as providers, our hands are occupied during that process. We’d like to free our hands to tend to other necessary tasks while ensuring the airway stays open.”
The MEA’s longer length tubing keeps the soft pharyngeal tissue beyond the base of the tongue open without the need for physical positioning like chin lift and jaw thrust.
Other advantages of using the MEA include:
The stiff plastic of traditional oral airway devices can cause sore, scratchy throats and difficulty in swallowing. The McMurray Enhanced Airway is made from soft, flexible materials, reducing potential injury to the oral cavity. Its longer and thinner tube ease placement and a built-in cushioned bite block also decreases the risk of dental damage.
The MEA is designed to open and maintain a patient’s airway and provide ventilation by opening the distal tissue beyond the base of the tongue. “The MEA addresses the clinical need of stenting opening pharyngeal tissue,” said Roxanne. “To accomplish this, sometimes people resort to workarounds—for example using a nasal airway orally, which occurs fairly often according to our research. That’s not what nasal airways are designed for and patients can dislodge or bite through the thinner nasal airway tubing if it’s placed in the mouth. The MEA is designed for oral use and it delivers the benefits of easy placement and the ability to keep the airway open without chin lift and jaw thrust maneuvers.”
The MEA’s external flange keeps the device securely in place. An optional connector can be coupled to an anesthesia circuit or manual resuscitator so that oxygen can be delivered closer to the lungs and away from the surgical area, helping reduce fire risks or provide intraoral positive pressure ventilation.
Unlike traditional oropharyngeal airways, the MEA is flexible and easy to insert. No lubricants or tongue depressors are required. The MEA’s ability to reduce or eliminate chin lift and jaw thrust is not only useful for patients’ comfort, but providers as well. “Holding a patient’s head in firmly in one position is hard on providers. I know from personal experience that your hands can become very sore,” Roxanne noted. She has been pleased with how her anesthesia colleagues have reacted to the MEA. The response to the MEA from users has been positive”. In a pilot study, more than 86% said the MEA would improve airway management and patient outcomes.
The MEA has proven valuable in several healthcare applications. In outpatient surgeries and procedures, and NORA cases, the MEA is an excellent airway management option for patients under deep sedation, many of whom are at higher risk for upper airway obstruction due to age, obesity or sleep apnea. It also helps maintain a patent airway when a mask might not work well—for bearded patients, for example.
The MEA is a good option for emergency personnel, too, as it’s small, portable and doesn’t require extra materials like lubricants or tongue depressors for insertion. For emergency responders who are not certified to places supraglottic devices or intubate patients, the MEA provides an effective means of keeping the airway open in addition to providing positive pressure ventilation.
An unexpected benefit during COVID is the MEA’s contribution to maintaining physical distancing to the extent possible. Because chin lifts and jaw thrusts aren’t required with the MEA, it can help reduce prolonged patient-provider physical contact.
For Roxanne, who is passionate about improving patient care and outcomes, decreasing healthcare costs, and healthcare innovation, delivering an important new solution for anesthesia has been very rewarding. “Our goal is to keep patients breathing, and I’m glad to help my colleagues and the patients they care for do that in an effective way,” she said.
To learn more about Roxanne and MEA, you can listen to our podcast interview here: https://outcomesrocket.health/mcmurraymed/2021/04/.
According to the 2020 Centers for Disease Control and Prevention report, roughly 34.2 million Americans have diabetes,...
Read MoreAs a farmer, Rod was used to long days. He worked 18 hours a day, 7 days...
Read MoreWith investors receiving hundreds of pitch decks every year, how do you create a compelling presentation that...
Read More
Brittany Busse Co-Founder, President, and Chief Medical Officer at
ViTelHealth


Stephen Thorne Founder and CEO at
Pacific Dental Services

Keith Carlson Nurse Career Coach