 | hosted by Joseph Kim
| hosted by Joseph Kim
“Decentralized Clinical Trials is a stupid term”; that’s right, we said what had to be said!
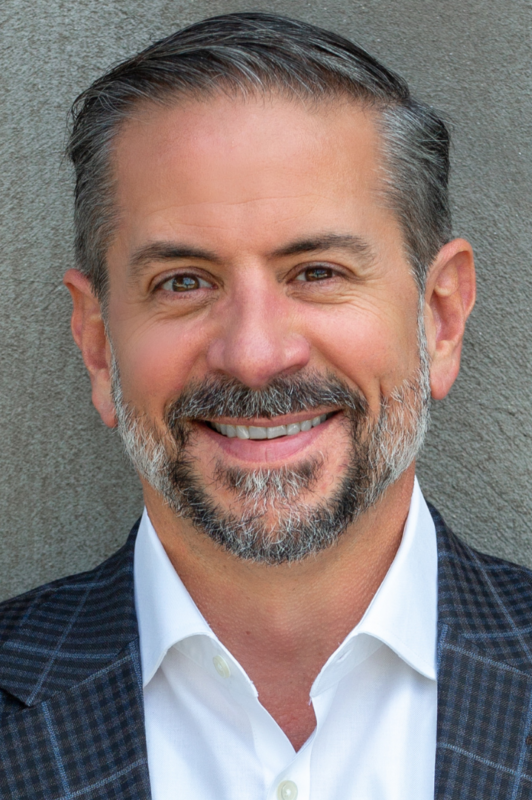
In this episode, Jeff Kinglsey, Chair, and CEO of Centricity Research speaks of what he loves about working in medical research and shares his opinion on decentralized clinical trials. He fell into the research world by accident and fell in love with the work he saw, admiring how much respect and attention patients got. Healthcare research has evolved a lot during the last two decades, increasingly incorporating technologies that facilitate patient participation. “Decentralized Clinical Trial” is the hot term right now, but Jeff doesn’t like it. He explains why Direct-to-Patient Clinical Trial would be a better term for what companies are doing with DCTs and gives insights into the benefits and challenges of doing clinical trials in this way.
Tune in and listen to Jeff Kingsley talk about his passion for clinical trials and how he’s working to revolutionize the research industry!
Dr. Jeff Kingsley is Chair and CEO of Centricity Research, an integrated research organization (IRO), with 40+ integrated clinical research offices across the US and Canada. Centricity conducts phase I through IV research in nearly every medical specialty; inpatient and outpatient; pharmaceutical, biotechnology, and medical device. Dr. Kingsley is also the founder, past Chair, and COO of hyperCORE International, a research site integrated network that has approximately 100 offices in five countries. Centricity and hyperCORE are changing the dynamic between sites and sponsors to serve sponsors in a way never achieved by sites in the past. He has dedicated his career to clinical research since 2006.
You can reach out to Dr. Jeff Kingsley at 706-536-6619 and jeff.kingsley@centricityresearch.com
Research Confidential_Jeff Kingsley: this mp3 audio file was automatically transcribed by Sonix with the best speech-to-text algorithms. This transcript may contain errors.
Joseph Kim:
Welcome to Clinical Research Confidential! On this show, we highlight and demystify the inner workings of this greatly misunderstood activity called clinical research. Now, why is clinical research important? Well, it’s the basis for nearly every modern remedy for sickness and a growing method to build trust and solutions meant to optimize health. But it’s not for the faint of heart. And so on this show, you’ll hear what it really takes to succeed in the clinical research game. I’m your host, Joseph Kim, and I’ve spent over 23 years in the clinical research industry, now serving as the chief strategy officer for ProofPilot. Get ready for some adventures as we look into the underbelly of clinical research.
Joseph Kim:
Hi, everyone! Today I’m here with the great Jeff Kingsley, who’s a provocateur in many ways, a clinical research professional. You’ve done a lot of your education in Pennsylvania, just like I have, degrees in biochemistry and biology, you did your medical training at Peckham, just down the road from where I am. He is the CEO of Centricity Research, and also a board member of ACRP, so lots going on there, Jeff. It’s been, it’s great to have you. Welcome to the show.
Jeff Kingsley:
Yeah, wonderful being here, thank you.
Joseph Kim:
So let’s start with your, let’s start with, like, how you got into research because like you, when you go into, you get a degree in biology and biochemistry, clinical research and drug interventional research isn’t like the forefront of your mind. So walk me through that sort of early career progression, how you first landed in research.
Jeff Kingsley:
Yeah! So honestly, it was an accident. I was aware of research going on in my residency program. I did bench research before I went to med school. I was interested in research from the start, but then took the traditional path from going through med school. In residency, there were people, specifically in interventionals, doing research and intensivists doing research. And so I was aware of what was going on in the hospital and it intrigued me. I didn’t participate in that, I wasn’t an investigator, but I read their protocols. I wanted to know what was going on in the hospital, I had interest, I was at least engaged. I was a family medicine physician and I had patients who couldn’t afford their own co-pays. I was writing prescriptions and I didn’t really know if they were actually taking their prescriptions as prescribed. They might be taking a daily medicine every other day to make it last twice as long. I started getting into research as a way of giving free healthcare, it’s really that simple. A friend of mine and I started a research company on a dime, very little work behind it. It was meant to be a way of delivering free healthcare. And we said, if we can just make enough, enough revenue from doing the research, we will take care of anybody who comes in the front door. Whether or not they qualify for a research trial, we will take care of them for free, we just need to have enough research revenue to keep the lights on. That’s how it started, and six months later, for six months, I had a foot in both worlds. So I’m seeing patients in standard of care, healthcare, and I’m seeing patients in research, side by side. And for six months I fell in love with clinical research. The amount of respect that we give to patients. They know from day one, in a very detailed informed consent document, exactly why we’re doing this, why we think it’s worth doing, how many visits they’ll have, the length of every visit, what will happen at every visit. The known side effect profile, an incredible amount of respect from the patient. We have more time to educate, completely free to the patient, and in fact, now we’re paying them for their time and travel. And so six months into this hobby, a way of delivering free healthcare, I fell in love with it, and I gave up my healthcare career and went full-time research. That was a couple of decades ago.
Joseph Kim:
That is a fantastic story, I’ve never heard a story like that. In fact, what I hear most often is research is not healthcare, which I think is a false kind of binary definition. Research is research. Now, of course, you’re not there to take care of the patient, but by definition, if you need a nurse and a doctor there, there’s some kind of healthcare going on.
Jeff Kingsley:
Yeah, yeah. Totally true.
Joseph Kim:
Yeah, Yeah.
Jeff Kingsley:
If you think about it, phase one is more science than healthcare, but two, three, and four are more healthcare, or I mean, two and three are probably balanced healthcare science, and four is certainly healthcare more than science.
Joseph Kim:
Yeah, absolutely. So you were always intrigued by looking at certain protocols and whatnot. What made you take the first, the first dip in like, all right, I’m doing this research as PI?
Jeff Kingsley:
My first real protocol was way harder than I ever should have been awarded. The sponsorship had said no, I apparently made a compelling argument. I had a fledgling company with almost no employees and I got a, twice daily, BID IV infusion, antibiotics study for really sick patients with moderate-to-severe skin, and skin structure infections. And so we’re, a trial like that, you’re dosing patients at 7 a.m. instead of p.m. You need a pharmacist, you’ve got blinded personnel that are mixing, you’ve got sleeves on top of the IV tubing, there’s a lot of complexity that kind of a trial. And in the early days, I had like four employees. Like I was not really equipped to do a trial like that, but that was my first study award and we simply staffed up for it. And, I mean, in the early days, I was easily there 14 to 16 hours a day and just loving it, just taking care of people for free and the good old fashioned way, you know? Oh, I loved it.
Joseph Kim:
Yeah, yeah, and, you know, we’ll get to this notion of remote trials and decentralized trials, but I think you’re laying down the groundwork of really what makes research rewarding for both the investigator physicians and the patient, which is this really strong human contact. And having been in trials myself, most recently two of them, a vaccine trial and glaucoma trial, there’s something real there. I did enjoy, like a virtual trial that one of the first research kit studies with Stanford, and like it enrolled very quickly, but I dropped out pretty quickly, too, because guess what? There was no one there holding me accountable, there was no relationship. So what you’re saying is, is a really strong foundational piece of clinical research I think people kind of forget is important.
Jeff Kingsley:
I think the bonds, the bond between a patient and the delivery of healthcare research is stronger in the research side than it is in normal healthcare. We’re, I was just saying, I did a state of the company event to the company yesterday, two days ago. And I was explaining to the company, in normal healthcare delivery, there’s no respect. You come in as a patient, you might be waiting in the waiting room. They might call it a reception area, but it’s a waiting room and you might be waiting there for 45 minutes. And then you get the privilege of moving from there to an exam room where you’re going to wait longer and then eventually you’re going to spend 8 minutes with a provider. There’s, the lack of respect in normal healthcare really bothers me, and it’s so much better in the research world.
Joseph Kim:
Yeah, and you know, it’s not the fault of the doctor, right? The system just forces it to be that way to some degree.
Jeff Kingsley:
Healthcare, it could, I mean, I was faculty in a residency program, and I used to teach residents how to see a patient in 8 minutes or less, so that you can see four patients an hour, including time for documentation, writing labs, and writing prescriptions, etc., four patients an hour, and that’s what healthcare economics dictates. So it’s not that doctors aren’t caring, but the economics of healthcare delivery these days dictates that you can’t take terribly much time with each patient, and it’s a shame.
Joseph Kim:
They can’t afford to care as they want, probably.
Jeff Kingsley:
Absolutely true.
Joseph Kim:
But, you know, this is starting to creep into the research world a little bit because protocols are getting more complex, right? So the amount of people you can actually see probably is going down. So walk us through like you did one protocol once. How many are you doing now? Like how big is your research practice?
Jeff Kingsley:
Oh, big! Today, Centricity Research has 43 offices across the United States and Canada.
Joseph Kim:
Amazing.
Jeff Kingsley:
We have about 600 concurrent trials going on today, in this area. I mean, we do research in intensive care units, inside of ORs, inside of ERs, and then, of course, the bulk of it is outpatient, but cardiology, nephrology, pulmonary, everything that you can imagine.
Joseph Kim:
Yeah, that’s a huge, that’s two orders of magnitude, more than when you started. Now, how do you scale that? Because these protocols, I mean, the first one sounded pretty difficult, but I have to imagine these later ones are more difficult than the ones you had ten years ago, right? Tell us a little about the difference.
Jeff Kingsley:
Yeah, we continue to specialize, more often than not, in the difficult trials. We tend not to do very much phase four because we’re not really designed for that. That really belongs inside of a physician’s practice who’s not really set up to do a lot of research. We’re created, we’re scaled, we’ve created a platform to do phase one, two, three, and so we do the highly complicated stuff. In phase one, we do glucose clamp trials and all sorts of things like that. But that is really, really our sweet spot.
Joseph Kim:
Yeah, yeah, and, how many different technologies are you using now?
Jeff Kingsley:
Are you kidding?
Joseph Kim:
What’s the average? Is it like 12 on average? I forget what the number is.
Jeff Kingsley:
Per trial? You know, I mean you can’t even possibly actually maintain your usernames and passwords for every piece of technology years in these days. I mean, the number of devices, let alone web pages, cloud-based technologies that you have to use on every single research trial is quite daunting. We’ve had some consolidation, as you’re well aware, over the years. You figure, you know, 15 to 20 years ago we were doing CRS on triplicate paper, right, where you had to use a ballpoint pen and press …
Joseph Kim:
I remember.
Jeff Kingsley:
And then we started moving into electronic solutions, cloud-based solutions. And in those early days, as you remember, there were lots of solutions. So you might have one trial with that tech vendor and another with that one and another with that one and another with that one, and you had to have usernames and passwords to each one, and you weren’t good at using any one of them because you had to use all of them, and then we saw a lot of consolidation in that space. So in that space now we have a couple of dominant players, which means that now you can sign on to a platform and you have maybe 24 trials on the same platform and you know exactly how to use that platform. So actually efficiency goes up and quality goes up in a lot of these other spaces around patient data collection, you know, e-Pro and the like. We still have lots of players in the space, which makes life harder for the site. You have that many more usernames and passwords, but that’s just the tip of the iceberg. The bigger issue for me is that when you have to be adept, maybe in air quotes, “adept”, at using all of these different platforms, the reality is quality goes down and efficiency goes down because you can’t actually be good at knowing how to efficiently use 14 different platforms.
Joseph Kim:
Yeah, I mean, what I’ve heard from study coordinators all the time is, okay, I have, I don’t even know when I need to use these things because they’re just sort of, there’s nothing kind of stitching it all together. So just, just knowing when to access each one is in and of itself a hurdle. Not because they’re stupid, but because there’s so many and there’s not a good guide for them.
Jeff Kingsley:
Sure, and sponsors and CROs, to this very day, will send you an email saying, oh, I need you to sign on to EDC and sign off on blah, blah, blah, blah patients, and they don’t actually tell you what trial they’re talking about they don’t tell you what EDC platform they’re talking about. It’s as if they assume you’re only doing their trial, so, therefore, you know all of this information. But if you’ve got 600 concurrent trials, I mean, what a waste of time for me. Now I’m like, now I have to like search through emails to figure out are they are these …, are they like, what? What? And so that, again, is just adding waste to the process.
Joseph Kim:
And so now we are talking about things like decentralized trials. And I’d like to quote you from Scope 2022 back in February, and you said very publicly on stage, Decentralized Trials is a stupid term. And you, I was in the room and you got a mix of applause, gasping, and sort of dead silence. It was a very mixed reaction, but I loved it all. Like, tell me what you meant by that. Let’s unpack that.
Jeff Kingsley:
Yeah, yeah, absolutely. I mean, we used to call it virtual clinical trials, and that’s not a good name because it implies it’s not a real trial and it absolutely is a real trial, so that wasn’t a good name. FDA kind of settled on decentralized clinical trials, which I hate the name. One, we’ve been decentralized for 15 years. I mean, that’s not new. We’ve been decentralized for a very long time, and it doesn’t speak to the purpose. Is the purpose to be decentralized? Is that why we’re doing this? Is there some magical reason why being decentralized is going to benefit the industry or the planet and all of humankind? No. The purpose is to move research to the patient. Call it direct-to-patient research. Direct-to-patient tells the patient exactly why we’re doing this. This is, it tells the entire industry why we’re doing this. We’re doing this to move the research to where you are so that we can collect data in your living room, in your place of work, to lower the burden of patients’ ability to enter research trials, and to eliminate the geographical barriers, which are huge.
Joseph Kim:
Yes, of course. I mean, I don’t, you probably remember, but this was 20 years ago when they started to do like the Hamilton Depression scale over the phone and we called, remember calling that centralized rating, although today we would call that decentralized. So it’s a really, it’s a silly term that doesn’t describe really what’s going on, and to your point, why we’re doing it.
Jeff Kingsley:
Who’s been anybody, why we’re doing it, which is really the critical thing. We’re doing it to reach out to the patient, to go to them.
Joseph Kim:
Yeah, and so, like you said, there’s been a lot of at-home components we’ve been doing for 15 or 20 years, whether it’s a simple e-diary or some other thing you can do at home, or home health nurse, those companies have been around forever. What, in your mind, defines, let’s just use the term, defines a decentralized trial from a non-decentralized trial? Is it the fact that one piece can be done at home or is there a threshold?
Jeff Kingsley:
I think it’s increasingly a subjective difference because when you think about it objectively, as you just said, for 15, 20 years we’ve been collecting patient, information from the patient. Increasingly over the course of time, we started with e-Pro, we used to have banks of cell phones that we would hand to the patients that they would take home with them. Then we started moving into tablets and we started moving it to then use your own device where you could download an app and the patient’s recording data, and now you’ve got obviously a massive increase in wearables. So over the course of all this time, functionally we’ve been increasing the amount of data collection, not centralized. Data collection, in the patient’s home, while they’re driving their car, in their workplace, and so, and we never called it DCT. So now arbitrarily, we’re saying this is traditional research and this is hybrid and this is DCT. And it’s like what? Which really fits in which bucket is kind of where you want to put the trial in which bucket. Now, obviously, if you’re 100% direct-to-patient, if the patient never has to come to a brick-and-mortar facility, then that clearly is DCT.
Joseph Kim:
Right.
Jeff Kingsley:
But the variations beyond that, we are collecting in all trials, 100% of trials today, we are collecting a ton of data outside of a research facility.
Joseph Kim:
And like, in terms of complexity, because that’s kind of where we have we transition to this. How much more complex is a trial with DCT components in it that are, I guess, more than just like the one e-pro component where people want to now do home health nurse, bio sampling, and e-pro? Like how much more complicated is for you as a brick-and-mortar site to accommodate that and also then be responsible as the PI, right?
Jeff Kingsley:
I don’t think it’s terribly more complex. The trial itself is no more complex. Trying to think, if I can believe what I’m saying.
Joseph Kim:
I love it.
Jeff Kingsley:
The trial itself is no more complex, it’s the same. The increased complexity comes in running business operations, clinical operations. That’s where the complexity comes in, and it’s not all that overwhelming. So, for example, if you’re doing a DCT trial where, let’s say a home health nurse is going to be going out to that patient’s house and they’re going to draw blood and they’re going to do a physical exam, verify that the tablet is transmitting to the cloud, whatever the case may be. The complexity comes in, really, a well-defined communication plan between the research principal investigator and the home health nurse. You know, if you go out to Mrs. Smith’s house and Mrs. Smith says, oh, by the way, last week I got into a car accident. I went to the ER, they kept me overnight, I was fine. Okay, maybe a normal life, that’s fine, but in research, that sounds like an SAE. So, you know, now the home health nurse just got this information. How does she communicate to the principal investigator in well, under 24 hours? You know, what if it’s a Saturday, a Sunday, what if it’s the 4th of July? Well-defined communication plan. And then who’s going to do what from there, is the home health nurse getting the record’s release to be able to contact the hospital to get the medical records? Who’s filing the SAE paperwork? And so you have to work on all of that structure well in advance of the protocol starting. Running the protocol in a DCT model is relatively just as simple as in any other model. The complexity comes in understanding who does what by when, when you have more people on the team.
Joseph Kim:
Got it, so the science isn’t more complicated. It’s all the little nits and gnats and the behaviors that are much easier to done under one roof, which is like, hey, Dr. Kingsley, this just happened, and then everyone knows what to do and they can jump into action because they’re in earshot of each other versus someone who’s hired by a different company altogether. And then how do they connect the dots? I got it.
Jeff Kingsley:
Yeah, absolutely.
Joseph Kim:
So orchestrating a lot of these behaviors and communications and, you know, interdependencies is going to be really the paramount issue when it comes to DCTs.
Jeff Kingsley:
Absolutely, it’s well worth doing. You know, many times we don’t do things because, well, why not do that? Well, because it’s hard. Well, that’s never a reason not to do something that’s worth doing. Yeah, I get it, it’s hard, but if it’s worth doing, do it anyway. And I think DCT is really that. The hardest thing we do in research is find patients that meet criteria for trials, by far, it is the hardest thing we do. And so anything we can do to remove that barrier so that we can engage with more patients who meet criteria for research trials is worth doing, even if it’s hard.
Joseph Kim:
Yeah, I mean, in recruitment, I’ve often seen, even in very successful campaigns, something like phone tag, just, you lose a lot of volunteers because of phone tag. And I get it, right? Coordinators are too busy. A number comes up, they don’t, patient doesn’t recognize it. Patients are busy. That’s a huge problem. Is it’s still a problem? It’s like a perennial thing.
Jeff Kingsley:
Still is, absolutely.
Joseph Kim:
Yeah, yeah, yeah. Let’s talk a little bit about sort of the fairness, not the fairness, that’s probably too provocative of a word, I won’t lead you, but once you have all these different people in decentralized trials, who’s in charge of paying them? Is it, because in a brick-and-mortar model, it’s very simple, right? The check gets cut to the clinic and then you guys deal with your PNL. But in a decentralized, when you have three, four, or five different parties executing things, how does that actually work? Are you, have you been exposed to some models? Do you have a preference, a priority? What do you think?
Jeff Kingsley:
At the end of the day, your compensation in doing DCT is going to be the same regardless of the model. What you end up with is a function of what you got paid and what it costs you to deliver your services. So you could have a sponsor that pays a research site, and the research site hires the home health nursing company and the phlebotomist and all this. And so your top-line revenue is going to be higher and all of your expenses are going to be higher because you’re paying all of these other vendors. Your net profit is going to be exactly the same. You can have a sponsor that wants to do it, a contract with the site, a contract with the Home Health Agency, a contract with a phlebotomist, a contract with a shipping company. The site’s top line is going to be smaller. The expenses are going to be smaller. Your net profit is going to be exactly the same. There are lots of ways of doing it when it comes to the ways of contracting to do DCT, but the bottom line is it doesn’t really matter because your profitability on doing the work is going to be identical no matter which way you slice it or dice it. So I really wouldn’t fret over that. From my perspective, I would accept any way that gets it across the finish line. If the sponsor is more comfortable doing all the contracts themselves, cool. If this sponsor wants me to do all the individual contracts, I can do that just as well.
Joseph Kim:
Got it, yeah, so as long as it’s fair, transparent, it doesn’t really matter to you. But, you know, fair and transparent can be hard to do.
Jeff Kingsley:
Well, it can. I mean, you have to be playing on the same team. You have to be able to play well in the sandbox with each other. You have to be able to be open and honest about what your actual expenses are so that people can trust one another and understand that no one is taking advantage of anyone else. And that’s, I mean, that’s what we should always be doing, no matter what. I mean, that’s, we’re not, fundamentally, we’re in research to change the future of healthcare. If that’s why you’re doing it, well, then remove all the friction from the system. Get through contract and budget as fast as you can, get steady, start-up as fast as you can. Enroll, the way you said you were going to enroll, collect high-quality data, hit your timelines, get database lock. And so similarly in a DCT model, be open and honest because it helps us get to a yes. If we start quibbling with each other, we’re going to end up not even doing the trial because we can’t get along. We can’t get the home health agency to trust that they’re being paid adequately compared to whatever the total budget is for running the trial, and that’s a loss for everybody, it’s not worth it.
Joseph Kim:
I love this, Jeff. You know, I pegged you as a cynic, but you’re a dreamer.
Jeff Kingsley:
Yeah, true.
Joseph Kim:
I love it. Thank you so much for spending time with us today. I have one final closing question for you. Now, you have plenty of runway left in your career, right? You probably haven’t even peaked. What keeps you motivated to keep progressing and growing Centricity Research and some of your other endeavors with the research community?
Jeff Kingsley:
Revolutionizing research, absolutely, absolutely. I say to the team all the time, doing research is a completely honorable career. It is a wonderful way to spend your time. You are giving an immense gift to the entire planet. You are changing the future of healthcare. We keep plaques on our walls of all of the FDA in the US, all of the FDA approvals that it was our data that got that, that made that happen. You’re changing lives well into the future, completely honorable. Revolutionizing research is actually choosing to make your life a little bit harder. You’re not just doing research, but you’re actually spending time, investing in technology to make it just incrementally better so it happens faster, more efficiently. That’s what keeps me excited about research, is the ability to continually invest in the industry and figure out how do we make it even better. Because there’s loads of opportunities you and I both know. The research industry, I love it, but we’re silly. I love the research industry and we are literally the arm of healthcare in innovation and we’re afraid of innovation. We’re slow to adopt technologies that are used by the banking industry today. We’re slow to adopt technologies that we can look at it and know that it would benefit our industry, blockchain, but we are slow to adopt things that could benefit. That’s opportunity for future growth. That’s what keeps me engaged in the industry.
Joseph Kim:
Yeah, fantastic. And the corollary question is like, if something were to go wrong, how is that going to happen, right? In terms of research, just kind of like stubbing its toe or, you know, blowing up a nuke in our face kind of a thing, like what do we, if we go wrong, how is that going to happen, do you think?
Jeff Kingsley:
You know, we’ve got lots of checks and balances in the research world today, which is a very good thing to prevent a nuke from blowing up in our face. Are we going to make mistakes? Sure we will. Are we going to, I mean, right now our industry is great at adding things. So this is another thing that makes me chuckle. Maybe chuckle is a little subdued for what I really wanted to say. We’re in the industry of running research. Well, how do you do that? You have a hypothesis. You say, well, how would I prove or disprove this thing? And then you run a trial and then you look at the data and you go, was I right? Was I wrong? What do I do next? And in running research, running companies, the business of research, we hear a sales pitch on a new piece of technology and we go, that sounds like it makes sense. And you sign a contract and you adopt the technology and you go, we never, I mean, we’re in the research world and we never actually go, how would I know if adopting this technology actually moved the needle to increase efficiency or whatever the case? And then I’m going to test it again in six months and find out. And if it didn’t make life better, we’re going to cut the contract and we’re going to stop using this technology. And so we tend to add things without ever testing, and then removing the things that didn’t work. We don’t really run the research business the way we run research trials, which is really comical.
Joseph Kim:
Yeah, this is brilliant, like for some reason we don’t use our research brains … We stop using, we adopt new things, but it’s precisely when you want to use it again.
Jeff Kingsley:
Yeah, so in terms of the things that can go wrong, if we can get better at analyzing what we’re doing, you make a change, it’s based upon sound data to say, this should work, and then let’s test it. And if it didn’t work, stop doing it, start doing something different.
Joseph Kim:
Yeah, no, I love it, this is great. Jeff, this has been such an inspiring talk. I really, really loved everything you said. Are you going to DPharm? Will I see you there?
Jeff Kingsley:
I won’t be at DPharm this year, I don’t think. I simply have too many trips coming up.
Joseph Kim:
Yeah, well, I’m putting a panel scope together, so maybe you’ll be up for that in February.
Jeff Kingsley:
Absolutely, let’s go, yes.
Joseph Kim:
Yeah, okay, well, I’ll reach out to you. Hopefully, your dance card isn’t too full. Thanks again for spending time with us, Jeff, this has been fantastic. And maybe we’ll have you on again because you’re such an entertaining guest.
Jeff Kingsley:
Sounds wonderful, thank you very much.
Joseph Kim:
Yeah, have a great day.
Jeff Kingsley:
You too, take care.
Joseph Kim:
Thank you for tuning into Research Confidential. We hope you enjoyed today’s episode. For more information about us, show notes, transcripts, and resources, please visit ProofPilot.com. If you’d like to debunk a clinical research myth, share some war stories, or maybe just show our audience what kind of heroics it takes to pull off gold-standard research, send us your thoughts, episode ideas, and more to help@ProofPilot.com. This show was presented by ProofPilot and is powered by Outcomes Rocket.
Sonix has many features that you’d love including upload many different filetypes, collaboration tools, automated translation, secure transcription and file storage, and easily transcribe your Zoom meetings. Try Sonix for free today.

