Moving the needle using advanced virtual reality
Episode 155
Thanks for tuning in to the Outcomes Rocket podcast where we chat with today’s most successful and inspiring health leaders. I want to personally invite you to our first inaugural Healthcare Thinkathon. It’s a conference that the Outcomes Rocket and the IU Center for Health Innovation and Implementation Sciences has teamed up on. We’re going to put together silo crushing practices just like we do here on the podcast except it’s going to be live with inspiring keynotes and panelists to set the tone we’re conducting a meeting where you can be part of drafting the blueprint for the future of healthcare. That’s right. You could be a founding member of this group of talented industry and practitioner leaders. Join me and 200 other inspiring health leaders for the first Inaugural Healthcare Thinkathon. It’s an event that you’re not going to want to miss. And since there’s only 200 tickets available you’re gonna want to act soon. So how do you learn more. Just go to outcomesrocket.health/conference. For more details on how to attend that’s outcomesrocket.health/conference and you’ll be able to get all the info that you need on this amazing health care thinkathon that’s outcomesrocket.health/conference.
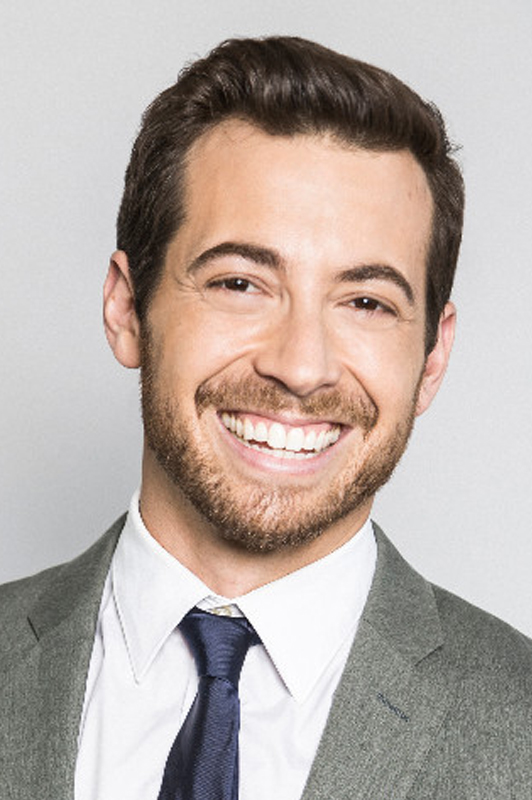
: Welcome back once again to the outcomes rocket podcast where we chat with today’s most successful and inspiring health leaders. I welcome you to go to outcomesrocket.health/reviews where you could rate and review today’s podcast because we have an outstanding guest for you today. His name is Dr. Justin Barad. He is an orthopedic surgeon and founder and CEO at Osso VR. They’re doing some pretty amazing things. His passion is medical technology. He’s always been fascinated with ways that software and tech can be applied to help people and as a pediatric ortho surgeon. He’s had an incredible way of just tackling some of the most challenging musculoskeletal issues facing our world’s children. And he’s got some technology to pave the way to do it as well. So I want to open up the microphone to Dr. Barad, Justin and have him round out that introduction. Justin welcome to the podcast.
: Thanks Saul, it’s really awesome to be here your show is fantastic. And thanks for the very kind introduction.
: Absolutely. You’re doing some pretty cool things Justin and I’m glad you’re able to carve out some time in your busy schedule. I always like to go to the root and wanted to ask you why did you decide to get into medicine to begin with.
: Oh wow. I mean if you really go back there was a computer game called life and death. They didn’t get me initially interested in medicine. Ironically it was sort of like a surgical simulation game. It was very primitive. I was really excited to be a doctor. This is I don’t know in elementary school probably like sixth grade. Then I went to a hospital once with my cousin who was a surgeon and I got very freaked out and decided did not want to do that. And mentally I took that the other direction and decided I want to become a videogame developer. So while I have been coding my entire life and I worked at Activision walls in high school I have a game credit with them which I was very excited about. And as I was finishing up high school kind of medicine came back into my life a little bit. Family member started becoming ill was in and out of the hospital. She’s fine now but it just made me realize that kind of what I wanted to do with my life. I wanted to have an impact and and maybe I saw a lot of challenges that she was facing that the healthcare system wasn’t necessarily equipped to deal with. And I thought to myself I wondered if there was a way to use software and technology to help solve medical problems. So in college I studied bioengineering at UC Berkeley with the goal of being an engineer inventor type in inventing technology. So as I was nearing college graduation I was interviewing for a bunch of jobs but nothing seemed quite right. It was like you know you were going to be kind of on that conveyor belt and helping increase efficiency of medical device production. So a gastroenterologist who happened to be my mentor Dr. Henry Lee and I sat down with him and you know he saw that I was kind of not very happy and he’s like well if you could do anything what do you want to be doing and I said I want to be inventing technology that helps people with medical issues. And he said well in order to invent something you need to know what the problem is and in the medical world the best way to find out what the problems are is to be on the front line as a physician. And so at first I said absolutely not. I don’t want to spend that much time in training but you know eventually he convinced me. So I spent a year in his lab doing research and getting all the pre-requisite classes and then I got into UCLA for medical school and I end up graduating first in my class and then I stayed there to do orthopedic surgery.
: Very cool. Very cool. So it’s just been this ebb and flow between medicine and programming video games. Kind a back and forth. And now you’re in this sweet spot where you’re combining both of your passions and interests.
: Yeah well I think we all have serpentine life and career journeys and when it kind of comes together in those Venn diagrams intersect that it can be a really special moment to know that everything you did sort of might have a purpose or a meaning. So it was during my training where I was experiencing what I thought was the most critical problem I’ve ever seen in medicine and that’s how we train our surgeons. And I was seeing every day how it just was no longer working at the level we needed to. And I saw a lot of patients being put at risk while people were basically practicing on them instead of knowing what to do ahead of time. And I was still very involved in gaming on the side and make monster games and experiment with new technology. And one thing I was very passionate about very early was virtual reality when I had this sort of renaissance after a brief attempt in the 90s in the field Virtual Boy which I still think is a fantastic system I love it. And so I got involved in the very early and I was able to hack together an oculus DK one which was the original Kickstarter release with this discontinued motion controller your hands and what that allowed you to do is get your hands into the VR experience which was really hard to do back then and wasn’t really an option. And the second I saw that I knew that I had found the solution for this problem. And initially I was like wow I can’t wait for someone to use this to solve this problem and then I had this kind of slow realization I was like wait a second I have this background to gaming. Maybe that person is me. So that’s kind of the the origin story of Osso VR. You know I started working on it on the site and building a prototype and then eventually met my co-founder who had quit professional gaming to pursue serious VR in October 2016. We both worked full time with the endeavor.
: That’s awesome man and listeners. You could hear the passion in Justin’s voice. And now if you go to ossovr.com. You’re going to see what they’re up to. You’ll find a link of that in the show notes as well as well as the other things that we’re going to touch on today. But super interesting capturing the essence of virtual reality and helping train both surgeons and also companies sales reps in these procedures. Can you tell us a little bit about what you think Justin should be a hot topic on every health leaders agenda.
: Well I think training should be at the forefront of everybody’s agenda as you say on. It is we’re in the midst of a training crisis and I think very few people realize this when you just look at some of the numbers. It’s very concerning. So to understand the surgical training process you know what you’re expected to do as a surgeon is you go to college is about four years typically in med school which is another four years. That’s 8. And then you have about five to seven years of residency. So then you’re looking at 13 or 15 on top of that and then typically another one to two years of fellowship. So a massive investment of time and money.
: Logn road.
: And a study came out in 2017 looking at the ability of graduating surgeons to operate independently. So you would expect that the end of all that someone should be able to do the job they were trained to do. And as of 2017 for the most common procedures 30 percent of graduating surgeons were unable to operate independent.
: That’s a big number. Yeah and it did talk about why.
: Yeah there are a lot of factors going on. It’s a phenomenon we’re calling sort of generally calling the training gap and it’s really pretty simple math. At the base of it in that the number of procedures we need to learn is always getting larger. Think about it. There’s new technology new approaches new techniques constantly new things that you need to learn. And in general newer techniques like minimally invasive techniques navigation technologies patient specific devices robotic surgery these are generally more complex and harder to learn than traditional open surgery. And compounding this problem is the time we have to train. So it’s actually becoming much less a few years ago. There were what were called work hour restrictions imposed on residents.
: I remember when that happened they kept it at 80 hours or something.
: Yes it’s kind of hilarious because people views it as very weak for only being able to work 80 hours a week. But it’s still quite a large number. But when you look at the difference between how many hours people were hands on with patients before and how many now that actually factors into about a year of training time. So it did have a big impact even though it’s the right thing to do because people were getting in car accidents on the way home post call was really terrible situation.
: Yeah.
: And then technology in a way is further affecting the issue because electronic medical records systems now take up a lot of our time. And so basically the people who are training us want nothing to do with the system so it’s typically up to the residents and fellows to be entering all the data and coding the counters. And research has shown that up to 50 percent of our time in the hospital can be spent on a computer on an electronic medical record systems and not in front of patients. So that’s another big factor.
: It is yeah, that so bad. And I don’t know what the answer to that is just and to be able to decrease the amount of time that spent on those things. I have a friend that started a software company and it basically is designed to make EMR easier and automate repetitive inputs and we need more more stuff like that. But anyway to get back on track here definitely a big problem. And so that also takes away from training hours.
: Exactly. And then I guess the final factor is sort of a shift in kind of the culture of what residents can or are expected to do and some of this is sort of a societal thing where we as a society are now more aware of residents and surgical trainees and very specifically say we would not like them touching us which is understandable but who are they going to touch and practice on and also focus on sort of efficiency and productivity of the operating room and also liability issues. So you know when you’re a surgeon and this patient is trusting you to get the very best care it’s hard to let someone you know is less skilled than you actually do parts of the procedure. And so it’s a bit of an ethical conundrum. So all of this combines to this dynamic which is very worrisome which is further worsened by the fact that there’s data showing that by 2050 we’re going to be about 50000 surgeons short because we have an aging population. We have a relatively decreasing workforce because we have this sort of like Demmink aging demographic that’s flipping in terms of the peer man and it’s leading to what’s going to be a very challenging dynamic where this population needs a disproportionate amount of procedures that kind of this relatively limited younger population cannot provide which isn’t helped at all by the fact that the vast majority of residency spots in the U.S. are subsidized by Medicare. And so the number of residents we can train is also fixed by the government. So a lot of challenges and really very little being done about it at the moment. And so you know I view a lot of what my job is not only in terms of providing a solution but sounding the alarm and educating people about the issue both in the medical and outside the medical world. I think we all as a society want people who are highly trained to be taking care of us and our greatest times of need.
: Yeah that’s that you bring up some really great points highlighted some big issues that we have in the system and let’s zoom into Osso VR and and Justin. Can you share a time or an example of how your organization has improved outcomes.
: Yeah. You know I didn’t leave full time surgical practice to kind of make a buck. I really want to solve this problem and so very early I wanted us to make sure that what we were developing actually worked and wasn’t just a cool marketing gimmick. So we did a small pilot study at UCLA and we took a group of medical students and half of them were assigned to VR training and then half were assigned to traditional training which was like a lecture textbook and some illustrations and things like that. Then we had them all individually go through and do we call it sawbones which people tell me sounds hilarious but it’s kind of like the closest you can get to actually operating on a patient. We had them all do a sawbones procedure and the blinded observer rated their performance. What we found at the end of that was that the VR trained individuals performed nearly double as well as the non VR individuals. So we have a lot more studies coming out of UCLA that we’re designing right now. And ultimately it’s very challenging but we want to tie use of our platform with how patients do in terms of complication rate length of OR readmission and things like that because ultimately you really want to show that this is directly affecting patients and their outcomes. But there is no doubt that the level of skill transfer you get just from a few minutes in VR is exponential compared to traditional means. So why would you want to know some of the surgeries that I participate in. We’re like 12 to 15 hours long. Why would you spend an entire day when you can learn exponentially more by doing yourself in just a few minutes as opposed to just standing around and watching. Which is what you do for the vast majority of these like five to 10 years of your postgraduate training.
: Yeah that’s a really good point fifty percent betters a big number and just thinking through all the things that could happen by way of variation there’s variation in the way that things are taught. There could be a more standardized and streamlined way to spread the training as well. Right.
: You touched on one of the key issues in the surgical world that everyone just does whatever they feel is best for the patient and there is zero standardization. And so if there is a way that we can all agree as sort of a professional group that here is the way that we want people to do this procedure it unlocks a lot of potential in that now you can actually measure how well that is working and make changes on a mass scale as opposed to just letting everyone do their own thing and hope that it works out well.
: Yeah that’s really interesting. And you know what I think would be really interesting to Justin if they took this product and you went to the board of you know orthopedic surgeons and and they incorporated it as part of becoming board certified.
: That is exactly what we are attempting to do.
: Is that right. Because I mean that right there is I think cementing it into the process. And they’ve been pretty receptive.
: Everyone I show this to as you know knows that this is something that is not a nice to have but a need to have and that we’re at sort of a crossroads and we really need to make investment in this area in order to solve a lot of the problems we’ve been discussing and that’s why we were able to you know assemble an advisory board of just unbelievable people like the former chair of surgery at Stanford in the presence of a very large professional societies so we’re really working you know not only to solve the problem on a technological level but also on sort of a regulatory and professional society and standard setting to agree on what do we want people to learn by the end of their residency so that you kind of know what you’re getting at the end of this machine to give you an example of why that’s not happening right now. Residency is really an apprenticeship training model so you’re just kind of following people around and just seeing whatever they walks in the door that day. So what happens is that just based on statistics you get a lead variable experience. For example one of my co residents was doing a hand surgery rotation and one of the most common procedures we do is a Distel radius fracture it’s a wrist fracture Mitz trauma. So it only happens when someone trips or the skateboard or accident and in his two months that he was doing this rotation where he’s supposed to see a lot of these you actually saw zero because they just never came in. Then he moved on to a different rotation and he just was never going to get that experience because of random chance.
: Interesting yeah that’s so true the trauma right if you focus on those particular things how can you augment it, it’s a good solution.
: Yes. So in Brian George’s paper from 2017 which I mentioned earlier about residents not being ready to practice. He sees this as a vicious cycle. So what’s happening is that surgeons are graduating they’re not yet able to practice on their own so they’re still learning. And so now they’re in practice with residents of their own. They’re expected to teach but instead of teaching residents they’re focusing on their own learning and then.
: Right.
: The cycle continues and worsens and so he thinks that one of the main ways to break this and create what’s called a virtuous cycle is through simulation which you’ve been seeing in aviation for decades be very effective in terms of you have a standardized curriculum that everybody needs to know so that their skill level is kind of a proficiency where they can perform the most common procedures safely and also have a launch pad to when they do get in front of patients. They’re starting from a more advanced level so they can get more out of their rotations. So in a worst case scenario like my co-resident at least he would have been proficient in the simulator. So he knew that it was safe for him to do that surgery out in the field as opposed to starting from zero which is what’s happening right now
: Totally yup and I’m just like envisioning it being part of you know hey you’re trying to get a fellowship here. Well can you show us your Osso score.
: Oh my God. You bring up one of the most incredible issues. I mean I think would blow anybody’s mind if they ever just looked into this. So I mean I would ask the audience like how much assessment of actual technical or surgical skill happens when someone is admitted into residency.
: Yeah I mean I don’t know what the answer is what is it.
: It’s zero. So typically it’s just you know if you have good grades and you seemed like a nice person you won’t mind being up with at 3:00 in the morning when neither of you have slept your end. And then at that point it’s almost impossible to get kicked out of the system like you could be a terrible surgeon but unless you’re actively murdering people which I assume it’s just you’re going to get all the way through. And so there’s some people aren’t be Olympic athletes or some people that can’t be pilots much like surgeons but these people just just get through and then you know they’re taking care of patients. And should they be are. And also you know this is an issue just down the road like what if you just can’t let yourself go and you’re just not really trying anymore. Don’t we want our surgeons to be of a certain quality level as a society and there’s just no one checking that are looking into that right now and you just can’t just coast through. It’s pretty crazy to me actually.
: Now it’s really interesting Justin and I think the direction that you guys are headed is definitely one that will potentially create as Standard a certification an index so to speak.
: Exactly I think people right now you know when I’m going to see a physician or one of my family members they’re really going on to things like availability and affability and the least important you know people say is ability but when you think about it there’s no way to really know that. Like what are you basing that off. It’s like what patients did well. Well actually most people do do well. The complication rate between like a really poor surgeon and a really good surgeon is a few percentage points so it may be hard for you to differentiate that you’re not going to get that out of Yelp reviews or anything like that. So I don’t think it’s it is a little unfair to patients that they’re not able to get some high level kind of indication of truly how deft is this surgeon how shaky are his hands right. Aren’t these things that people want to know.
: Oh totally. Yeah. So it sounds like things are going well. Justin can you share with the listeners a time when he made a mistake or had a set back and what you learned from that.
: Oh wow. So so many I would say you really want to hiring I think is the biggest challenge when you’re starting a new company in a new endeavor. And the tendency is to want to just build the team build the empire and just when someone comes along maybe you’re having trouble attracting technical talent and you just need somebody. But I would caution people that I think team trumps talent really and there is like a fit and you want to. In the early days it’s just so crazy that you need people that you’re going to be able to be honest with work well you know practice radical honesty as they say. And just stay focus with ruthless prioritization and the concept of like too many cooks in the kitchen or just throwing more people at it doesn’t necessarily lead to more productivity or a better solution. So you know stay lean iterate quickly and really just I would say that the biggest word for us has been focus. You’re doing something no one has ever done before. You can go in any direction you want. And so I think the tendency is to try and go in every direction sort of spray and pay or spaghetti against the wall and just see what sticks. And there is some of that that has to happen. But if you have focus on a vision and really stay mission driven and so like have a North Star or like what does everybody working towards. I think that has gotten us through I would say ninety nine percent of our challenges. Whenever we have an issue with the technology customer just internally with our team we always remind ourselves why we’re doing this and what we’re trying to do and we’re able to find a solution and get through it and just you know being very careful that everyone we bring on feels that same way.
: That’s a great share. And listeners it’s all about the team you build and the focus in your why and the direction and Justin and his team definitely have a clear north star and they’re doing some really interesting things. So as far as I understand it Justin you guys are are looking beyond orthopedics you’re looking into cardiac procedures isn’t that right.
: Yeah. We’re exploring the robotics and interventional cardiology space as well and we’re really focused on areas where the complexity and the technology have gotten to the point where they exceed our ability to learn it in a reasonable period of time. So you know a lot of robotic technologies or some of these new structural heart procedures you may have to perform 50 to 100 times before you can do it safely and with the tools we have available today that’s mainly happening on patients. And so in something like the world of Cardiology I mean that’s potentially fatal event but oftentimes what happens is a surgeon or procedure list will try a new technology which is amazing for patients and they want and are typically higher value and have a bad experience very early on and they’ll feel burned by that. And in the industry they call it a one and done phenomenon. So what happens if a surgeon feels that the device is unsafe and not realize that they were just undertrained and they’ll stick with older technology which is probably not as good for patients. And so what we’re trying to do. You know one of our mission statement is increasing patient outcomes through the adoption of higher value medical devices and techniques and also democratizing access to modern surgical education around the world which is something you can do with our technology.
: I think that last piece is really interesting too because there’s countries around the world that don’t get the opportunities a lot of people that want medical training come to the U.S. because there’s a lot of great training here. And this is a way that people could actually get the training without even coming.
: Exactly. It’s VR has the power of what we say teleportation and capturing expertise and distributing it. And so even you know you have people from other you know very well regarded countries coming here to learn how we do things. But there is the world like where I go on medical missions where they don’t have the opportunity to travel anywhere or really get much training where they are and things that are very easily treated here like a lot of trauma that young people experience over there often goes untreated or mistreated and it’s a huge burden for their economy because they’ve taken a very young productive member of the economy and is no longer able to work because of sometimes a very minor injury. So this technology has the potential for really massive global impact in a way that I’m really excited to see and we’re really committed to that global mission.
: That’s awesome just and very inspiring when you guys are doing and it’s more than just here at home. What would you say one of your proudest medical leadership moments that you’ve had to date.
: Wow I still think just running a team and taking care of patients is something that I’m immensely proud of and I still think is the most special opportunity and it’s a real privilege to have someone in their time of need to depend on you and not only that but you’ll be able to deliver for them and to see people who are in horrific accidents walk again again are born with certain deformities and suddenly you know their legs are straight and they’re walking around. I remember there there was one patient when I was a resident. And he clubfoot is a very common congenital deformity that is present at birth and it’s treatable with just some casting and a very minor procedure and usually doesn’t cause much issues throughout life but it’s untreated. You’re basically walking on your ankles and it’s very very deforming and debilitating. So the 16 year old from Liberia came to Shriners Hospital was working at. We were able to do this in what’s called a salvage surgery where we kind of cut out a bunch of bones from his ankle and fuse it together. It’s not ideal but you don’t have a lot of options at that age. He’s coming back in for a follow up and I was walking by him and I heard him say like. He’s like dad dad that’s the guy who made it so I could walk again and I cry like every time I think about that. And that was a moment like that that I knew that I was doing something that I really want to dedicate my life to.
: And that the powerful just and you know just being able to touch patients in that way is a really powerful thing. Thank you for sharing a great story. Justin let’s pretend you and I are building a medical leadership course and what it takes to be successful in medicine. It’s the 1 0 1 course with Dr. Justin Iran. And so we’ve got four questions lightning round style followed by a book and a podcast that you recommend to the listeners. Ready.
: Very ready.
: All right. What’s the best way to improve health outcomes.
: I think the best way to improve health outcomes is through training I might be little biased and also assessment. So we have one part of the puzzle which needs a lot of improvement but we have none of the other we need to know how are practitioners doing technically so we can know what can they what should they and shouldn’t be doing and give patients access to this data as well. And I think that’s really what’s going to take us to the next level in terms of outcome. And it’s just a data set. Nobody’s looking at right now.
: Awesome. What’s the biggest mistake or pitfall to avoid.
: I think I see this all the time but I find problems and not solutions taking a solution from the tech world or an idea you have in trying to find an application within medicine is almost always going to be the failure. It really takes a deep deep understanding of a problem and the various stakeholders involved the regulatory and reimbursement pathways the path the commercialization the competitive landscape a level of capital required all of these things are very important but they all stem from a problem and not necessarily the solution that you’re thinking of. And so it really really really encourage people within medicine to just record problems and not necessarily ideas for like cool widgets. And if you’re outside of medicine I really encourage you to get inside somehow so shadow a surgeon holism some around and clinic volunteer just get in there get on the front lines. That’s what I did and it works wonders and every corner you’re going to face some sort of challenge some sort of pitfall. And the answer is not going to come from some new technological development is going to come from understanding of the problem and how to approach that problem from a slightly different angle or how to approach a different stakeholder that you have deep understanding of so practice need based innovation find problems avoid the solution rabbit hole.
: That’s a great call out. Justin how do you avoid eroding your impact. Despite all the constant change.
: I think just stay involved and build your network. It’s really easy. If you’re within medicine to just be siloed and just do it you do clock in and clock out and this bit which the world is moving now. You’re going to miss everything fly by you and suddenly what you do might not really be as effective or irrelevant anymore. And so it’s really important to stay connected to the world and whether that’s technology or policy or somehow do something outside of the day to day of medicine. And similarly if you’re interested in the medical world like I said stay involved and keep one foot in there so you can understand what are the shifting dynamics. What are the politics. What are patients saying it just going to make all of the difference and make you be able look one to two steps ahead. I always think about cardiothoracic surgery and how they were approached with interventional technologies and catheters and they felt that they didn’t need it because what they did was fine. What they didn’t understand is that their patients needed it. A cardiologist jumped at the opportunity and now cardiothoracic surgery is kind of a shadow of its former self. And you know cardiology is a booming field and so it’s stories like that that remind me that it’s really important to stay connected to your patients in the world of technology.
: Beautiful what would you say one focus area that every health organization needs to keep in mind.
: I would say to have more of a focus on fostering innovation. And I don’t mean like starting an innovation group but truly from soup to nuts training your workforce and your physicians to understand innovation and how to interface with the world of startups and large companies and outside of medicine and not just function within your silo once again. And I say this because I feel that innovation is really a lifelong discipline and it’s not something you can learn in boot camp or you know a few months at a seminar. And I think there really just needs to be a culture of innovation and it should be encouraged. And there should be policies that reflect that in order for an institution to really stay ahead of the curve and you know make sure that it’s kind of like this was born here we did this. We contributed to this world because surely a rising tide lifts all boats and you’re seeing this in the tech world all the time. It was really I had moderated a panel with a CMO of Samsung. And you know the medical director from Qualcomm was sitting right next to him and they both said that our companies sometimes don’t work together but we need are technologies to interface with each other in order for us both to be successful. So I feel like right now this message hasn’t really gotten across the medical world and you could certainly see it in the way that the EMR situation has manifested itself with the lack of interoperability. But the key is that if everything works together you get synergy an exponential increase in outcomes. And if everyone is just doing their own thing you’re getting just additive kind of like baby steps. And that’s not enough anymore with the rate of change in terms of the needs of the population and the exploding health care costs.
: That’s a great call. Justin and what book and what podcast would you recommend.
: In terms of books I would recommend Doctors: The Biography of medicine if you are interested in medicine and startups in any way you will find this to be a very inspiring book because it is the physicians who made huge leaps for our profession and for our society in terms of the health care they receive but also the stories behind them. Who were they as people and why did they take these huge leaps or dedicate these lives to what everyone else thought was crazy like a Andreas Vesalius who at the time Galen had determined that we had discovered all there is to know about medicine. And there was nothing else to know. And people believed him and no one ever questioned this for a thousand years and then Basileus from Pat came out and he realized that Yalan had never even dissected a human cadaver before he’d only done animals and that was very taboo at the time so in secret he started dissecting human cadavers actually realized that there were many many inaccuracies and basically overturned a thousand years of medical knowledge by him kind of being the original medical disruptor or rebel. And there are many many more stories in the book and I find it very inspiring because these people who are like the heroes of our profession there are just people and they had the same kind of problems that we do and it’s very relatable and gives you the idea that you do have the potential to solve these problems. Any one of us can do it. It just takes you deciding that I am going to do this. I’m going to stand up. I’m not going to wait for someone to tell me that I can or can’t help to solve this problem.
: Love it. What a great recommendation and what podcast would you recommend.
: In terms of podcasts. I’m going to go nonmedical here there’s this podcast called Song Exploder. I think it’s just totally fascinating. It goes over his songs and basically breaks out each individual track and you can see how it all interfaces together. It’s really interesting to see how these individual tunes that sound totally weird in isolation went together create a really incredible song. Kind of reminds me of medicine and surgery a little bit and I also love music so I highly recommend it when it’s really cool and different.
: Yeah you know. That’s on my ass subscribed list as well. Justin and listeners it is a very interesting podcast. Definitely check it out. Don’t worry about writing anything down. Just go to outcomesrocket.health/barad Thats that’s Justin’s last name. B A R A D. You can find all of our show notes as well as links to Osso VR and all the things that we’ve discussed above the podcast. All these things just and this has been incredibly fun. All good things have to end as well. So here before we conclude I’d love if you could just share a closing thought and then the best place where the listeners can get a hold of you or get in touch with you.
: I would just encourage everybody listening to this. Just I always say it’s okay to quit but never give up. I think the world is so exciting and you don’t know what is in store and the next step in your pathway. And so I always say just have a bias for action just constantly move forward. You never know when a random Stanton game development is suddenly going to become relevant later on or if the path you’re taking is the right one. Just don’t worry about that just keep walking down it.
: It’s a great message and what would you say the best place if somebody is interested in Osso or just collaborating with you guys how to get in touch.
: Yeah you can email me justin@ossovr.com or you can check out our website. There there’s a contact form there www.ossovr.com. We have a big initiative this year to partner with healthcare institutions all over the world and also medical device manufacturers to help get their technology out there.
: Beautiful Justin. This has been a ton of fun. I definitely know that the ideas you shared are going to help people improve outcomes and I thank you for that and hope to stay in touch.
: Likewise. It was a total pleasure
Thanks for tuning into the outcomes rocket podcast if you want the show notes, inspiration, transcripts and everything that we talked about on this episode. Just go to outcomesrocket.health. And again don’t forget to check out the amazing Healthcare Thinkathon where we could get together took form the blueprint for the future of healthcare. You can find more information on that and how to get involved in our theme which is implementation is innovation. Just go to outcomesrocket.health/conference that’s outcomesrocket.health/conference be one of the 200 that will participate. Looking forward to seeing you there.
Recommended Book and Podcast:
Doctors: The Biography of Medicine
Best Way to Contact Justin:
justin@ossovr.com
Mentioned Link:
Episode Sponsor:

