Let’s discuss the intersections between pain, metabolic health, and addiction.
In this episode, Gurpreet Padda, a seasoned pain management specialist, talks about his extensive background and his journey through diverse medical experiences, eventually focusing on pain management and the complex relationships between pain and social determinants of health. Pain is a symptom of underlying issues, and considering metabolic inflammation in effective pain management is something Dr. Padda has found to be extremely important. He touches on the challenges posed by the pharmaceutical industry’s influence and misaligned incentives within the healthcare system, highlighting the significance of tackling chronic pain, addiction, obesity, and metabolic health collectively. Throughout this conversation, Dr. Padda also delves into the origins of the opioid crisis, innovative pain management methods, and the critical need to incorporate metabolic and lifestyle factors into managing chronic diseases.
Tune in and learn more about the complexities of chronic pain management!
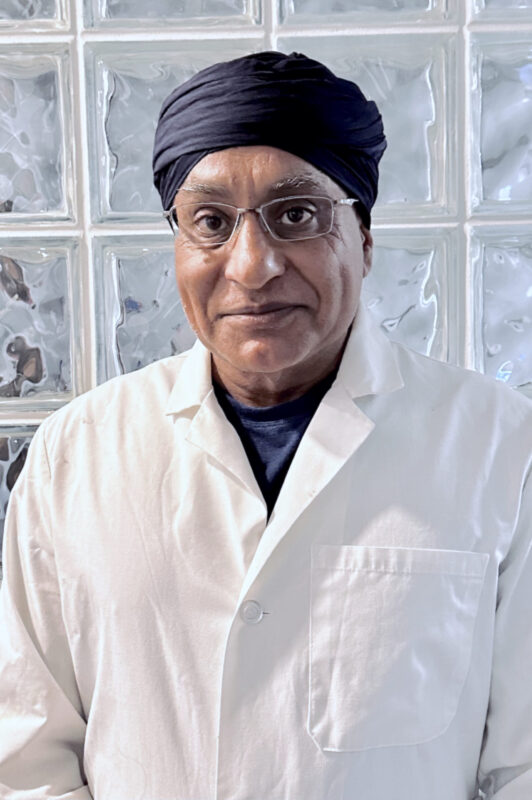
Dr. Gurpreet Padda is an esteemed physician with over 25 years of experience specializing in pain management in Saint Louis, MO. He graduated from the George Washington University School of Medicine and Health Sciences in 1992 and is affiliated with SSM Health Saint Louis University Hospital.
His holistic perspective has led him to explore the intricate connections between chronic pain, metabolic health, addiction, and social determinants of health. This perspective has driven his innovative strategies in pain management, where he strives to address the root causes and provide comprehensive solutions.
Download the “Chalk Talk Jim_Dr. Gurpreet Padda Part 1 audio file directly.
Chalk Talk Jim_Dr. Gurpreet Padda Part 1: this mp3 audio file was automatically transcribed by Sonix with the best speech-to-text algorithms. This transcript may contain errors.
Jim Jordan:
Welcome to the Chalk Talk Jim Podcast, where we explore insights into healthcare that help uncover new opportunities for growth and success. I’m your host, Jim Jordan.
Jim Jordan:
I’m very excited to have Dr. Gurpreet Padda with us today. Dr. Padda is a physician with over 25 years of experience specializing in pain management. He currently treats in the inner city of Saint Louis, Missouri. He has a unique background, having grown up in India before immigrating to the United States as a child, and this instilled in him grit and adaptability that has served him well throughout his multifaceted medical career. He completed his medical training through an accelerated six-year program and went to pursue surgery, anaesthesia, and ultimately, pain management. Beyond his clinical practice, Dr. Padda is passionate about addressing the intersections of chronic pain, metabolic health, addiction, and social determinants of health that underline them. He teaches and speaks nationally on a number of these topics with his holistic perspective and wealth of experience. I’m just simply thrilled to have him here. Thank you for joining us today, and please introduce yourself to our audience.
Dr. Gurpreet Padda:
I’m a medical physician, I, … of Saint Louis, Missouri. I have a tumultuous background because I wasn’t in the United States, I grew up in India. I grew up on the Pakistani border, and I was born about three years after Partition. So India had been just separated from Pakistan, and I grew up, and it was there was a lot of tribalism; there was a lot of issues associated with partition from Pakistan. Pakistan was waging an active battle, and India was as well. The British had just left and looted trillions of dollars, so they left us with no money and had destroyed the infrastructure of India, so we were pretty impoverished. And I came from a political family, and the family assist in Pakistan, and we were Sikh, and my grandfather was a freedom fighter, and my great-grandfather was a freedom fighter. I grew up in a situation where there had been fatwas or edicts declared against my family, so they were trying to kill the male heirs of our family. I happen to be a male heir of the family, and so there was always a constant risk of being poisoned or shot or killed. So I grew up having a Belgian Malinois as my sidekick, who was a police, it’s a military dog, and somebody walked around me all the time with a double … shot, and I kept trying to get food from …, because I’m a kid. And I looked at people, and I go, hey, what are you eating? And so I would taste that, and then somebody would run over and shove an emetic in my throat, so I would puke, so I hadn’t been poisoned. My family got tired of having to watch me so much, so they sent me to a location in Amritsar where nobody knew who I was, and people stopped trying to poison me. But that also meant for about 5 to 6 years, I didn’t meet my parents. And so, I grew up in an area where I could self-educate because I didn’t have a lot of parental supervision. I had horrendous ADD, even then, I knew that I had a problem, but I also was hyper-inquisitive by nature. And so that kind of gives you the background of coming from an area with tremendous amounts of crisis and having being forced to look at situations in a way that’s different. We would get air raids and literally get bombed, and we, I had codes that I had been told to memorize, just like little kids memorize prayers. I had been given codes to memorize so that if we got bombed, when we got bombed, I knew how to escape and get to a certain place. It was a train station at the third archway on the right, there was a bolt hole, and that’s where I would go hide, and somebody would come get me. So if I ever got separated, that’s where I would go. So that was the initial kind of chaos that I came out of. My parents are both pretty well educated. They decided that they wanted to get me out of India, and I didn’t really know who they were, but they picked me up one day from this boarding school, and before I knew it, I was in the United States, and I had, the school that I had gone to was Russian speaking because India was experimenting with communism and we all learned Russian. I didn’t know one word of English when I got to the United States, I could speak Punjabi, I could speak Hindi, and I could speak Russian, but I couldn’t speak English. So I was enrolled immediately in school, and I was in an all-black school as a brown kid wearing a turban, not speaking a lick of English, but at a hyper inquisitive nature, and did pretty well. Being from a communist place, I always wanted things, and I didn’t have a lot of resources because I was supposed to not have anything. And so when I got to the US, I realized what a great capitalist place this was, and like, you could get anything you wanted, and nobody like made you throw up if you got food from the street, and I was fascinated. So I quickly adopted to this concept of capitalism.
Jim Jordan:
How old were you when you came over?
Dr. Gurpreet Padda:
Nine, nine. And so I quickly started selling door-to-door greeting cards. And then I learned all kinds of valuable lessons because you don’t sell door-to-door greeting cards, barely being able to speak English, not understanding the economics of it, and sell these greeting cards for this magical thing called Christmas, and you’re selling these cards in September, and they’re customized to the person who’s buying them with their name. And by the time you drop them off in November, they don’t want those cards anymore, and you can’t sell them to anybody else but that name. So I quickly learned some business concepts and learned to hustle pretty early. Eventually, my parents moved us from the city to the county, and now I was a brown kid with a turban in an all-white school. And so, in both situations, I’d been able to study the people around me because I didn’t really quite fit in having that separation and coming from an area with a lot of crisis. And every time I heard a tornado siren in my head that went off as an air raid siren, and immediately, it created panic, and I live in the Midwest, and so we’d get tornadoes all the time. So it was a different kind of experience, and it maintained a separation, which was probably good. Because it allowed me to experience life as an outsider inside this country and realize how wonderful it was, like people just didn’t realize. Like for me, I was like, it was amazing. I couldn’t believe all the things that people in America had access to that I never had access to. I quickly got into computers, I quickly got into construction, I quickly did all kinds of other things. By the time I was 14, 15, I was having people work for me, and I would, we would rehab houses. And so by the time I was 15, I would have my construction workers drop me off in the morning at school, and then they would call me in the high school cafeteria at the payphone to tell me how they were doing during the daytime, and at the end of the day, they’d pick me up, and we’d go to the construction site. And so I loved that aspect of it, I loved the hustle of business. I loved science, I love computers. So I eventually ended up in medical school, a six-year program. By the time I graduated, I’d done a lot, and I loved medical school, it was the coolest thing ever. I would purposely take extra call. I would take every night call whenever I could just to get the experience of that because I’m an adrenaline junkie, I would want to be there if a trauma showed up. So I wanted to do surgery, I wanted to do everything I could. If there was an interesting pathology case, I would volunteer to go to see the autopsy because there were only about 7 or 10 autopsies a month that were being done, and you just never got that kind of clinical experience unless you actually volunteered, so I would volunteer all the time because I really loved it. I saw one of the first HIV patients in Kansas City in the mid-80s, in 1985 or so, and I was convinced the patient had psittacosis because he had a bird and no one had heard of HIV. And here we are in the middle of the night doing a … on this guy who ended up dying the next day and getting hacked up and coughed up red blood and all kinds of stuff, and this was before personal protective equipment and all of this stuff, so it was an interesting experience, and I’m attracted to that adrenaline concept. So eventually, at the end of medical school, I decided that I hadn’t taken any time off because it was a six-year program and it was done in one-month blocks. And so I had saved up all my vacation, and I knew I had to do something in public health. So I took what residual vacation I had left, and I took my public health, and I went to Australia and did a rotation treating Aborigines off the north coast of Australia. And it was really cool because I was the doc, and it was the end of medical school, and I was the doctor, and there wasn’t another doctor. And so I got to deliver babies, and treat STDs, and fix bones, and this was up on a coastal island, so there was no way to call for help, and so it really, it made you learn how to do that. And at the same time, I got to do a really cool stuff, like I learned how to scuba dive, and I learned how to do other things. Got out of medical school, went into surgery at Cook County Hospital in Chicago, because, again, I’m an adrenaline junkie, but I burned out a little bit because there was the great nursing strike of 1988, 1989, and all the Filipino nurses left, and here I was trying to figure out how to do chemotherapy infusions on cancer patients that were also surgery patients. I had no idea what I was doing and ended up spending like a couple of months in the hospital, never leaving. By the time I got out, went out to my car, and there were homeless people living in it, and they’d taken everything. And so that was when I realized that maybe I should do something else because I like some freedom of time. And so I realized that the anesthesia residents would go home at night, and I wasn’t going home, and so I decided I’m going to do anesthesia, and besides that, I was getting bored of the mechanical aspect of things. So I went into anaesthesia and I love Neurophys, did that and ended up in pediatric anesthesia eventually, then ended up in pediatric pain, then ended up in adult pain and went through the university programs and was academic for a while; got fascinated again by business because it was a recurring loop for me and worked with all kinds of companies working on capital, migration, and things of that nature and trying to, and in between I’d gotten an MBA in finance and was doing international finance. At the end of it, I ended up graduating, was fascinated by research, eventually migrated from anesthesia to pain, and have been doing pain since, and that’s where I’m at now. I’ve been in the inner core for about 25 years doing pain management with a very difficult set of patients and trying to figure out how to help them. And in that process, I’ve learned all kinds of other things.
Jim Jordan:
How do you see pain management fitting in the continuum of healthcare in general?
Dr. Gurpreet Padda:
Pain is a symptom, and we all know that, pain is the symptom. It’s the symptom that tells you that something has gone terribly wrong. That’s how people have pain. People don’t have pain because, oh, I hurt my foot yesterday, and today it hurts a little bit, and then tomorrow it doesn’t hurt much. People have ongoing pain because they have something that has gone wrong. Our natural endorphin system has failed us, and our inflammatory system has failed us, and now we have unrelenting, terrible pain that’s not being mediated or treated by the usual biologics of endorphins and wound healing. So there’s something that’s gone wrong. And so as I was looking at my patients and wondering why is it that I can treat their pain and get them better, but then, and why is it, at the same time I’m looking at them going, why is it that these patients are like pretty overweight and they don’t have that much money? And I thought it took money to get food. And so, why is it that my patients are overweight, they have this chronic pain, and they don’t have much money? And that posited some interesting thoughts in my head, and I started researching that and looking at biometrics. At the same time, we had this epidemic of pain, we had this epidemic of obesity, and we started to get this epidemic of addiction. And I eventually ended up getting boarded in addiction and ended up getting an additional certification in metabolic health, and in the addiction side, I realized that it was more than just exposure to drug. It was more than just, oh, you give somebody a drug, and they’re addicted because not everybody that gets a drug gets addicted, only about 3 to 5%. So what about the other 95%? Why don’t they get addicted? And why is it that the rates of addiction globally are going up? And so these are all the questions that are going through my head, and I ended up coming to some conclusions. What I figured out was that the reason why we have chronic pain is we have severe metabolic inflammation. We have abnormal metabolism that is a necessary precedent to maintaining pain levels because we have severe neuroinflammation, we have insulin resistance, and those are necessary in order to maintain a pain cycle. And at the same time, because our culture is one of hedonic-driven drive, we’re constantly looking for something to activate our dopamine receptor, and it just so happens that opiates will do that very effectively, so will TikTok, and so will alcohol, and so will a whole host of other things. That’s why people have this addiction issue. And then it’s more than that because only about 5% of these people get really addicted, even though a lot of them are exposed. So it’s also a social determinant of health that impacts that, and that primary social determinant of health turns out to be loneliness. And so you have to fix that in your pain patients before, and your addiction patients, before you can unravel all of this. So I ended up basically in treating pain-addiction-obesity as an entity, as one common entity, because it all overlaps, and it’s called metabolic inflammation. And so I talk on that field, and I teach that field, and that’s how I manage and treat my patients. It turns out that’s about two-thirds of the united healthcare budget per year, two-thirds. So if you can fix that, which you can, two-thirds of the budget goes away.
Jim Jordan:
So say that again, two-thirds of the budget.
Dr. Gurpreet Padda:
US Healthcare budget is related to metabolic inflammation, and it’s a preventable disease. And the problem is that everybody wants, they want a pill, they want a medication to fix this. And you’re not going to fix it with a pill or medication, and because you’re not going to fix it with a pill or medication, you don’t have a pharmaceutical companies running out sponsoring studies on lifestyle medicine or improving metabolic health. And so the issue is that unless you fix that, you don’t fix pain, you don’t fix addiction, you don’t fix type-two diabetes, you don’t fix obesity, you don’t fix early-onset cognitive decline, you don’t fix the prevalence of solid tumors. There’s a whole host of cascades, and I talk on that, and I talk nationally probably six times a year, and I get invited internationally to talk as well.
Jim Jordan:
Given the fact that addressing social determinants of health doesn’t often yield direct financial returns for those product folks, coupled with the rise of digital health and data collection that may reveal cause-and-effect relationships, an important question arises. When this data becomes available, clearly showing the systemic costs and their impact, how will these issues be resolved if there’s no direct profit involved? Who will invest the resources in addressing these problems even when we have the necessary data? I understand this is somewhat a philosophical question, but do you have any thoughts on this matter?
Dr. Gurpreet Padda:
The answer is that the independent, self-insured corporations will force that issue. Medicare will force it indirectly, and they’ve been trying because they keep saying, quit doing procedures, and we’re going to not pay you on the basis of procedure, we’re going to pay you on the basis of outcome. The problem is that Medicare is a captured organization, and so they’re not paying on the basis of outcome, they’re actually paying on the basis of pharmaceutical companies who implant protocols into healthcare. They’re paying on the basis of what big agriculture has implanted into the dietary guidelines. If you look at the American Dietary guidelines, for example, they recommend a very high amount of carbohydrate, far in excess of what human beings need, and carbohydrates are not an essential element of our health. Fats and proteins are, but there is no carbohydrate that we need. We have something called gluconeogenesis. And so if we do need some carbohydrates for the red blood cells and we do need some carbohydrates for some limited brain structure, it’s probably less than 20 grams a day, we can produce that from the existing fat and from the existing protein that we consume. So we really don’t need any carbohydrates, and yet the food pyramid is 150g of carbs a day, which is supported by big agriculture and reinforced by the pharmaceutical industry that doesn’t want to give up the fact that we might be better off not taking statins and we might be better off not taking all of these other drugs. And if two-thirds of healthcare goes away tomorrow, the pharmaceutical companies are going to be in trouble. The incentive should be to get rid of this. The problem is that the agencies are captured. It’s called corporatism. It’s what Mussolini described during the Second World War, when the corporate interest is aligned with the governmental interests, and there’s a feedback loop that occurs, the only person that really suffers is the population, because as individuals, we don’t have that. So the only people that are really pushing hard, for example, Virta Health is doing a great job, but they’ve contracted with a variety of independent insurance carriers. Also the, there are other areas that might benefit from it, but the incentives are misaligned, like the Indian nations, the indigenous nations in the US have an independent healthcare system, but their incentives are misaligned. You think about it for a second. The number one cause of disability for firefighters in the United States is heart-lung disease because they’re overweight, but they all go out on disability with a presumptive disability diagnosis of heart-lung because they assume that it was from pollution, but it really is from the food that they were eating at their firehouse. So these are, but you can’t get the fire department to change because it would change their disability ratings. It would change how they went out on retirement after a certain number of years. And I’ve tried to do that, I actually have met with them here in Saint Louis and tried to convince them that we could feed them differently. We could have them lose weight, and we could document the change in …, document, the changes in LPIR, document the change in insulin, document their weight change, do a … score, show the … of calcium in the artery, and their coronary arteries, and all those things are doable, but the incentive is misaligned because, for them, the incentive is, I work a couple shifts a week, I go out on an obesity-related illness, and then I can get another job in my retirement, and so the incentive is fundamentally misaligned. It’s the same thing with the armed forces. The number one reason why people came back from Gulf War Two, the number one reason was not because they got injured in the war; the number one reason why people were repatriated from Gulf War Two was because of obesity-related illness.
Jim Jordan:
This has been a fascinating discussion so far with Dr. Padda. We covered the origins of the opioid crisis, innovative approaches to pain management focused on reducing the reliance on opioids, and the role of metabolic and lifestyle factors in driving chronic disease. I’m going to break this into two parts. So in part two of our conversation, we’re going to explore potential solutions, including overhauling dietary guidelines and properly aligning incentives in our healthcare system. We’ll also be discussing opportunities like leveraging artificial intelligence and data, so please be sure to tune into part two, and hear the rest of this incredibly insightful discussion on improving pain management and our overall healthcare system.
Jim Jordan:
Thanks for tuning in to the Chalk Talk Jim Podcast. For resources, show notes, and ways to get in touch, visit us at ChalkTalkJim.com.
Sonix has many features that you’d love including secure transcription and file storage, generate automated summaries powered by AI, enterprise-grade admin tools, powerful integrations and APIs, and easily transcribe your Zoom meetings. Try Sonix for free today.

